View this page in Welsh
Download the full report or read the summary of findings on this page.
What's on this page
Overview
In Wales, around 340,000 people are living with heart and circulatory diseases (also known as cardiovascular disease or CVD). With an ageing population, this could rise.1 Many thousands have risk factors for these conditions, which include hypertension, high cholesterol, type 2 diabetes and obesity.
Heart and circulatory disease accounts for more than 1 in 4 (or 27%) of deaths in Wales each year. This translates to around 9,600 deaths. Out of those, around 2,700 are people under the age of 75.2
Factors that impact cardiovascular health
Cardiovascular health is closely linked to broader factors that influence overall health. These include:
- income: a person's earnings and financial stability
- environment: a person's surroundings, including air quality and access to green spaces
- access to health services: whether a person can easily get medical assistance when needed.
What are health inequalities?
Health inequalities are differences in health status, healthcare and health-related risks between different population groups, that are unfair and avoidable.3 These include:
- health status: some groups of people may have a shorter life expectancy than others
- healthcare: some groups of people may find it harder to access healthcare services than others
- health-related risks: some groups of people may find it harder to access healthy foods than others.
Socioeconomic disparities that influence health
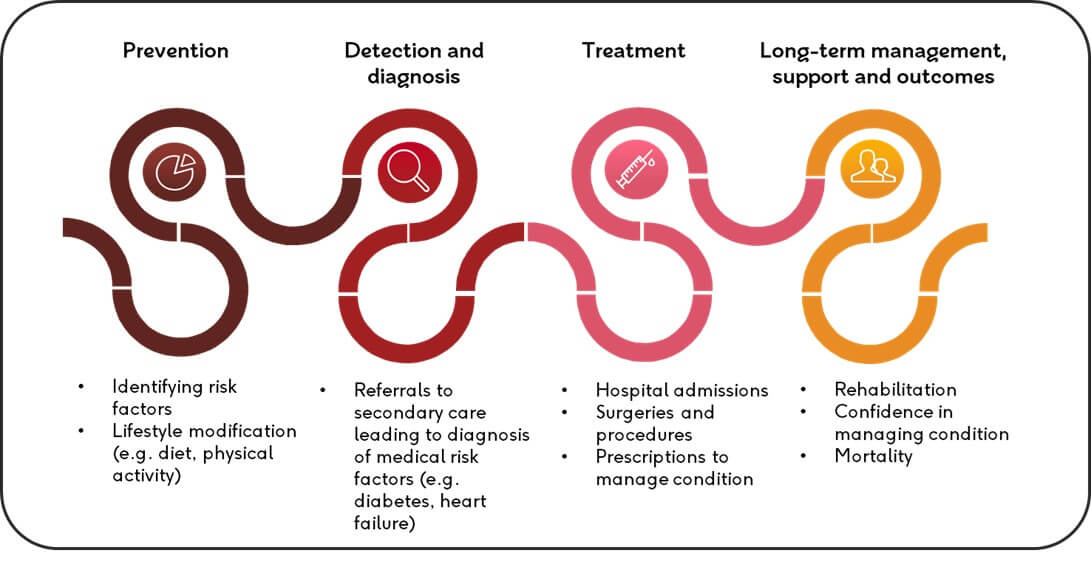
There are clear and consistent gaps between the most deprived and least deprived groups across the cardiovascular disease pathway in Wales. We can see this in:
- the prevalence of risk factors (i.e. the percentage of a group affected)
- the number of hospital admissions
- the management of healthcare
- health outcomes (especially early death).
The association between deprivation and cardiovascular risk factors
Heart health is influenced by several risk factors such as smoking, living with obesity or excess weight, diet, and alcohol consumption.
How common these things are in a population can be shaped by access to healthcare, social care and the conditions of where people live.
Key CVD risk factors in Wales
- Smoking: The prevalence of smoking in the most deprived groups (at 22%) is almost 3 times that of the least deprived (at 8%). Between 2020 and 2023, the difference in smoking rates between the most and least deprived groups has grown.
- Living with obesity or excess weight: Those in the highest deprivation group have a higher likelihood of obesity (at 32%) compared to those in the lowest deprivation group (at 22%). There has been a slight decrease in overweight and obesity rates from 2020 to 2021. But the gap in obesity rates between high and low deprivation areas has widened. The most deprived areas have a higher prevalence of excess weight and obesity (66%) than the least deprived areas (58%).
- Physical activity: There is a clear association between physical activity and deprivation in Wales. The most deprived groups in Wales are less likely to get the NHS-recommended 150 minutes of physical activity each week, compared to the least deprived groups. But the gap has narrowed between the most and least deprived areas – in terms of the percentage of adults getting at least 150 minutes of physical activity each week.
- Eating habits: We found a strong association between how deprived an area is and the percentage of people who reported eating at least 5 portions of fruit and vegetables in the previous day. In the most deprived areas, 22% reported eating at least 5 portions in the previous day, compared to 36% in the least deprived groups. Those in the most deprived group were also more likely to have not eaten any portions of fruit and vegetables the previous day, compared to the least deprived group.
Graph showing the prevalence of CVD risk factors in Wales, 2022/23
View the table data for this graph.
Prevalence and availability of healthcare
Our analysis used 2 different methods of examining the prevalence of CVD by deprivation in Wales (i.e. how common CVD is in the most and least deprived parts of Wales).
One method we used looked at what proportion of people self-reported having a heart or circulatory problem in the National Survey for Wales. This approach found that 11% of people in the most deprived group reported a heart and circulatory complaint, compared to 9% in the least deprived.
The second method we used revealed the opposite. In this approach, we categorised GP practices into 5 groups, based on the proportion of their patients who lived in the 20% most deprived parts of Wales. We then looked at the percentage of patients in these GP ‘clusters’ who were on their GP’s register for different heart and circulatory diseases, and high-risk conditions like hypertension. This approach suggested that CVD was slightly more common in less deprived areas.
The difference in findings in the 2 approaches makes it hard to determine the true association between deprivation and how common CVD is in Wales. Possible reasons for the differences are discussed in more detail in our full report. More research, and the provision of age-standardised prevalence data for Wales, is needed to better understand this connection.
Graph showing the prevalence of heart and circulatory diseases in Wales, 2022/23
View the table data for this graph.
Hospital admissions and deprivation
Cardiology admissions to hospital increased in Wales from 2020 to 2023, regardless of deprivation level. To look at hospital admissions by deprivation, we used data on GP ‘clusters’ – which are groupings of GPs determined by local health boards – and ranked these based on the proportion of their patients who lived in the most deprived parts of Wales. We found that the most deprived health board in Wales also had the fewest cardiology admissions.
Primary care
We also looked at the composition of the GP workforce and how it is affected by deprivation. This is important as GP practices play a big part in the detection, diagnosis, and management of heart and circulatory diseases, and their risk factors.
In 2023, there were more fully qualified GPs in the most deprived areas in Wales than there were in the least deprived areas. But the least deprived areas had more nurses and support staff (administration staff roles) compared to the most deprived areas.
The fact that there were more fully qualified GPs in the most deprived areas could be explained by these areas having greater health needs. But having comparatively fewer nurses and support staff could negatively affect the quality of patients’ healthcare experience in more deprived areas.
The cost of CVD prescriptions was also higher in the least deprived GP cluster.
Graph showing general practice staff volumes by staff type and general practice deprivation cluster, April 2023
View the table data for this graph.
Secondary care
Data for secondary care and deprivation in Wales is limited. However, when we examined cardiology admissions at the local health board level, we found that the most deprived local health board had a lower non-emergency cardiology admissions rate than the least deprived health board.
The impact of deprivation on death rates
There is a strong association between deprivation and CVD mortality, both for the all-age and under-75 mortality categories.
All-age CVD mortality rates went down from 2013/15 in the most and least deprived local authorities in Wales, until the beginning of the Covid-19 pandemic in 2020. Since the start of the pandemic, all-age CVD mortality rates have increased in the most and least deprived parts of Wales. This is with the exception of women in the least deprived areas (for whom rates have continued to go down).
Under-75 CVD mortality rates also decreased in Wales from 2013/15 until the start of the Covid-19 pandemic. However, since this time, early CVD death rates have gone up, mainly in the most deprived local authorities.
From 2013/15 to 2020/22, we’ve also seen the gap in premature CVD mortality rates between the most and least deprived local authorities increase (by 7 per 100,000 population).
Graph showing age-standardised mortality rates (all-age and under-75s) for heart and circulatory diseases in the five most and least deprived local authorities in Wales, from 2013/15 to 2020/22 (3-year average)
View the table data for this graph.
What needs to happen next
We need to see:
- that people are given the information and tools they need to manage their conditions and risk factors
- approaches to reduce inequalities at each step of the cardiovascular pathway.



