We’ve produced a report that provides
for the first time, a holistic understanding of health inequalities surrounding cardiovascular disease (CVD). It offers insight into the strengths in Northern Ireland’s health system as well as where improvement is needed across all areas of healthcare.
All contents reviewed and published November 2023. Please refer to our Northern Ireland factsheet for the latest health statistics.
Download the full report or read the summary of findings on this page.
What's on this page:
Overview
An estimated 225,00 people are living with heart and circulatory diseases in Northern Ireland today.1
Many thousands have risk factors for these conditions including raised cholesterol, type 2 diabetes, obesity, and high blood pressure. Heart and circulatory diseases cause nearly a quarter (24%) of deaths in Northern Ireland and a quarter of those people are under 75.1
Cardiovascular health is closely linked to broader factors that influence overall health. These include:
- Income: a person's earnings and financial stability.
- Environment: a person's surroundings, including air quality and access to green spaces.
- Access to health services: whether a person can easily get medical assistance when needed
What are health inequalities?
Health inequalities are differences in health status, healthcare, and health-related risks between different population groups that are unfair and avoidable.2 They include:
- Health status: e.g., some people may have a shorter life expectancy than others.
- Healthcare: e.g., some people may find it harder to access healthcare services than others.
- Health-related risks: e.g., some people may find it harder to access healthy foods than others.
Socioeconomic disparities that influence health
There are clear and consistent gaps between the most deprived (low socioeconomic status) and least deprived (high socioeconomic status) groups across the cardiovascular pathway in Northern Ireland. We can see this in:
- the prevalence of risk factors
- hospital admissions
- the management of healthcare
- health outcomes (especially premature mortality).
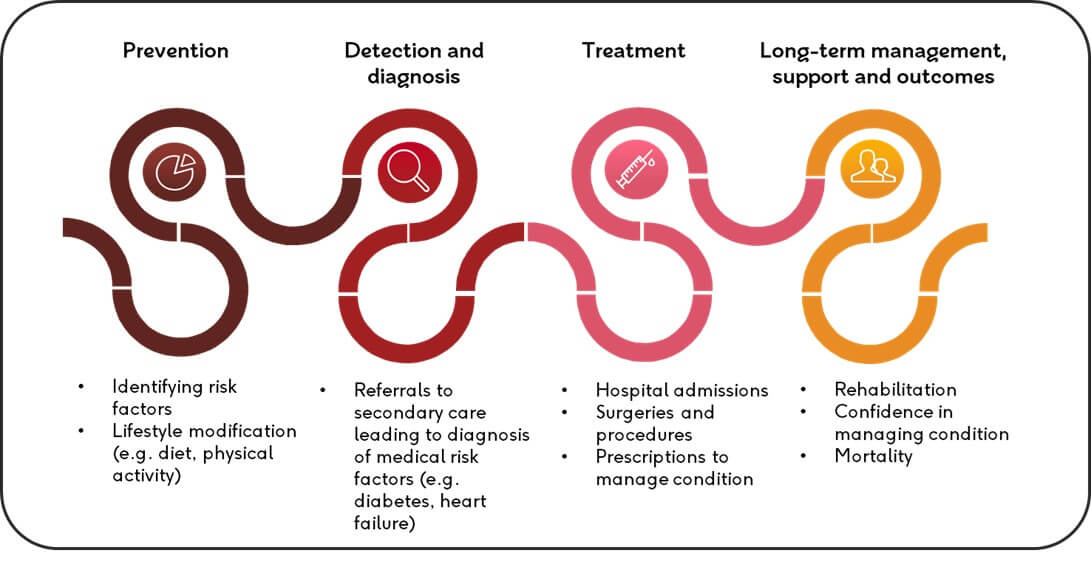
The cardiovascular disease pathway (CVD pathway)
The link between deprivation and cardiovascular risk factors
Heart health is influenced by a number of risk factors, such as smoking, obesity and overweight, diet and alcohol consumption.
How common these things are in a population can be shaped by access to healthcare, social care and the conditions of where people live.
Key CVD risk factors in Northern Ireland
- Smoking: In Northern Ireland, fewer people are smoking than 10 years ago. But people in the most deprived areas are 2 to 3 times more likely to smoke than those in the least deprived areas.
- Obesity and overweight: Since 2010/11, the proportion of people who are overweight or obese has been higher in more deprived areas. In 2019/20, 25% of people in the least deprived areas were classified as obese, while in more deprived areas it was 32%.
- Eating habits: In 2022/23, over half of the adult population in Northern Ireland said they ate less than 5 portions of fruit and vegetables in the last day (56%). But 42% of people in the most deprived areas ate at least 5 portions of fruit and vegetables, compared to 46% in the least deprived areas.
- Alcohol consumption: The relationship between alcohol and deprivation in Northern Ireland is complicated. In 2022/23, 19% of people in the most deprived areas drank more that the weekly alcohol limit. This surpassed the 17% in the least deprived areas. Notably, it’s the first time since 2011/12 that the most deprived areas have had a higher rate of drinking above the weekly limit than the least deprived areas.
Prevalence and availability of healthcare
Hospital admissions and deprivation
People living in the most deprived areas are more likely to be admitted to the hospital for heart and circulatory conditions.
Over three years, from 2019 to 2022, there were more hospital admissions in the most deprived areas (1,666 per 100,000 people) than in the least deprived areas (1,398 per 100,000 people). This trend is also seen in those aged under 75.
Graph showing heart and circulatory hospital admissions per 100,000 population from 2015-2022
There is also a table showing heart and circulatory hospital admissions per 100,000 population from 2015-2022.
Primary care and deprivation
In areas with the highest levels of deprivation, there are fewer doctors in primary care compared to the least deprived areas, with a difference of about 7 doctors for a population of 100,000 people.
The number of GPs in each local government district has changed in the last decade. From 2014 to 2023, all local government districts (LGDs) lost doctors except for one, with most
losing 5-7%. However, in one LGD, the figure was as high as a 29% reduction in the number of GPs.
Prescriptions and socioeconomic status
People in most deprived areas are more likely to get prescriptions for blood pressure (antihypertensives) and cholesterol (statins) medications compared to those in the least deprived areas and Northern Ireland as a whole.
This corresponds with British Heart Foundation’s CVD prevalence estimate which shows that the most and least deprived local government districts differ by 3 percentage points in terms of prevalence.
It’s important to note that no association was seen between deprivation and the prevalence of specific heart and circulatory conditions and the risk factors we examined.
Graph showing BHF CVD estimate in Northern Ireland by LGD deprivation rank in 2022/23
There is also a table showing BHF CVD estimate in Northern Ireland by LGD deprivation rank in 2022/23.
When examining specific heart and circulatory diseases and risk factors (Atrial Fibrillation, Coronary Heart Disease, Diabetes Mellitus, Heart Failure, Hypertension and Stroke/TIA) no real association is seen between the most and least deprived areas as well as overall.
Graph showing the prevalence of heart and circulatory conditions and risk factors by LGD deprivation rank in 2022/23
There is also a table showing the prevalence of heart and circulatory conditions and risk factors by LGD deprivation rank in 2022/23.
The impact of deprivation on mortality rates
From 2012 to 2021, the number of people dying prematurely from CVD in Northern Ireland has gradually decreased. This is good news.
However, those who are most deprived are still more likely to die earlier from CVD than those in least deprived groups.
Shockingly, the premature death rate for CVD in the most deprived group is more than twice that of the least deprived group. This highlights the strong link between deprivation and cardiovascular health outcomes.
Graph showing age-standardised death rate for under-75s for circulatory conditions from 2013-2021
There is also a table showing age-standardised death rate for under-75s for circulatory conditions from 2013-2021.
A note on Covid-19
The implications of the Covid-19 pandemic on cardiovascular heath inequalities are difficult to quantify.
Examining further data over time could give us more information. It’s likely that data collection in Northern Ireland was affected during the Covid-19 pandemic. In some cases, survey questions were not asked and in others the data sample collected was much smaller than in previous years. And often, less data was collected for more deprived groups.
What needs to happen next
We need to see:
- that people are given the information and tools they need to manage their conditions and risk factors
- health services connected with local figures who can engage with people in more deprived communities
- approaches to reduce inequalities at each step of the cardiovascular pathway.
Footnotes
1. Northern Ireland Fact Sheet, BHF.
2. This definition of health inequalities is based on similar definitions provided by organisations including: Public Health Scotland, NHS England, The King’s Fund, and the World Health Organization.



