What’s on this page
Blocked arteries explained
Your arteries are a key part of your heart and circulatory system. They carry oxygen-rich blood from the heart to organs and tissues around the body.
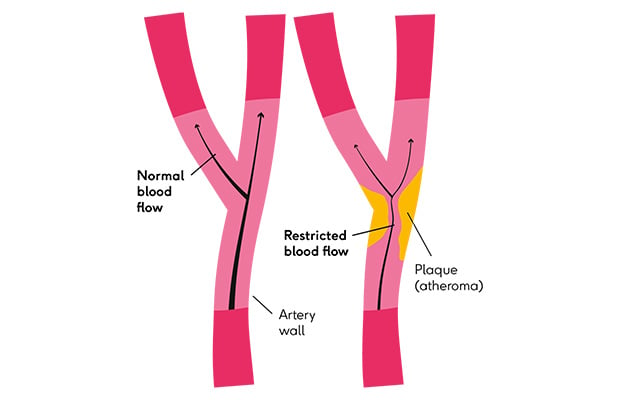
But if the walls of the arteries become damaged by something like high blood pressure, this can cause inflammation (your body’s response to injury) and can lead to the build-up of fatty material.
Your body tries to clear up the inflammation, which creates a seal of fibrous material over the fatty material. Over time, this forms a hardened plaque (also known as atheroma), making your artery narrower.
This process, known as atherosclerosis, gradually continues as more fatty material builds up. This can cause more inflammation and result in a bigger plaque, and a narrower artery.
Symptoms of blocked arteries
Plaques take a long time to build up, so people with clogged arteries may not have any symptoms for many years.
But once the plaque gets big enough, the artery can become so narrow that not enough oxygen-rich blood can get through. This can cause pain or discomfort, especially during exercise.
Coronary heart disease is when the arteries supplying blood to your heart (coronary arteries) become narrowed. Chest pain (angina) is a common symptom of coronary heart disease.
Or if the arteries in your legs are clogged, you may notice pain in your legs (claudication), which is a sign of peripheral arterial disease.
But the biggest risk is if the plaque ruptures (breaks off) and the blood flowing through the artery forms a blood clot around it, which blocks your artery.
If a blood clot forms in the coronary arteries, this will cause a heart attack. And if it happens in an artery supplying blood to your brain, such as the carotid arteries in the neck, it will lead to a stroke.
Want to get fit and healthy?
Sign up to our fortnightly Heart Matters newsletter to receive healthy recipes, new activity ideas, and expert tips for managing your health. Joining is free and takes 2 minutes.
I’d like to sign-up
Causes of blocked arteries
There are several things that can increase the risk of fatty material building up in the arteries:
- High cholesterol – this is a natural fatty substance carried around in your blood. If you have too much of the ‘bad’ type of cholesterol, it can build up in damaged areas of the artery walls.
- High blood pressure – if the pressure of the blood flowing in your arteries is too high, they can become stiff or narrow.
- Smoking – the chemicals in tobacco and cigarettes can make the walls of the arteries sticky.
- Diabetes – this condition can lead to too much sugar building up in the blood, which can damage the artery walls.
- Living with excess weight or obesity – this can increase your risk of high blood pressure, high cholesterol and diabetes.
Because fatty material takes a long time to build up in the arteries, getting older also means you have a higher risk. However, blocked arteries can still happen in younger people, especially if they have any of the risk factors above.
Tests for blocked arteries
If you are aged 40 to 74 and live in England, you can have a free NHS health check. If you live in Northern Ireland, Scotland or Wales, check with your GP about assessing your risk of heart or circulatory disease.
A doctor or nurse will assess your blood pressure, cholesterol and medical history to work out your risk of having a heart attack or stroke.
You can also ask to have your blood sugar checked if you have a family history of diabetes or any symptoms.
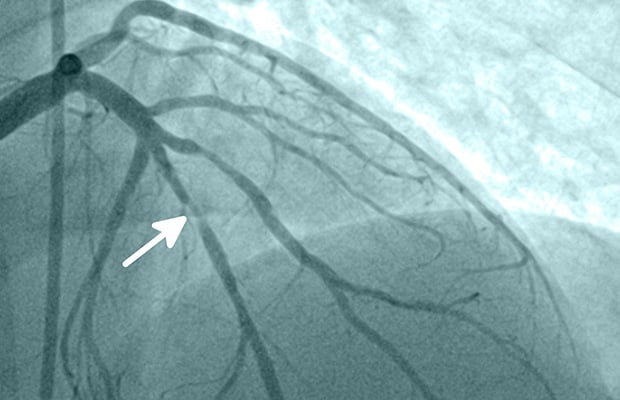
If you’ve already had a heart attack or stroke, or you have symptoms like chest pain, there are other tests that can see if your arteries are blocked or narrowed.
These include:
- Angiogram – a special dye is injected, and an X-ray is taken of your heart to see if there are any narrowed sections or blockages in the coronary arteries (pictured below).
- CT calcium score – a scan that measures the amount of calcified plaques in the coronary arteries.
- Cardiac MRI – a test that uses magnetic and radio waves to look at your coronary arteries.
- Doppler ultrasound – a test that uses sound waves to check blood flow in the limbs.
- Carotid ultrasound – a test that uses sound waves to check blood flow inside the 2 largest carotid arteries in your neck.
Treatment for blocked arteries
While it is not possible to unblock clogged arteries, there are ways to slow the development of plaques, widen the arteries and reduce the chances of a heart attack or stroke.
Medicines
Medicines can slow down how quickly fatty material builds up, protect the arteries and also prevent blood clots.
These include:
- Statins – to reduce cholesterol levels and reduce the risk of fatty plaques breaking off from the walls of your arteries.
- Anticoagulants – such as warfarin to prevent blood clots, often known as blood-thinners.
- Antiplatelets – such as aspirin or clopidogrel, which also prevent blood clots.
- Nitrates – to relax and widen the blood vessels.
- ACE inhibitors or ARBs – which can reduce high blood pressure.
- Beta blockers – to relax the heart. Some beta blockers relax blood vessels too, which helps to lower blood pressure.
Surgery
If you have coronary artery disease or you’ve had a heart attack, then you may be treated with angioplasty.
This is where a tiny balloon is inserted and blown up to widen the blocked artery. In many cases, a tiny metal mesh tube called a stent is put in place to hold the artery open after the balloon is removed.
If many coronary arteries are severely narrowed, you may need to have coronary bypass graft surgery. This involves a healthy blood vessel from a different part of your body being attached (grafted) onto the blocked artery so blood can bypass the blockage.
Significantly narrowed or blocked arteries in the legs or pelvis can also be treated with angioplasty and stenting, or occasionally bypass surgery.
Blocked carotid arteries in the neck can also be treated by making a small cut to the artery to surgically remove plaques or blood clots.
Lifestyle changes
Leading a healthy lifestyle and managing your risk factors is vital to slow down the build-up of fatty material in the arteries.
This will help to prevent symptoms such as angina and reduce the risk of having a heart attack or stroke.
This includes:
- Eating a balanced diet – try to eat more fruits, vegetables, wholegrains, beans and pulses, and fewer foods that are high in salt or saturated fat.
- Staying active – this will help you manage your weight and reduce cholesterol levels.
- Regular health checks – see your GP or nurse to have your blood pressure and cholesterol levels checked.
- Quitting smoking – this will reduce the risk of damage to your blood vessels.
Meet the expert
Professor Martin Bennett is a British Heart Foundation Professor of Cardiovascular Sciences at the University of Cambridge, researching why people develop atherosclerosis. He is also a consultant cardiologist and works at Addenbrookes and Papworth Hospitals.
What to read next...