

January: Harnessing the power of the immune system in heart attack recovery
2022 got off to a great start with news that a drug used to treat certain cancers could improve recovery after a heart attack and may become the first treatment of its kind available to patients.
A heart attack triggers cells in the immune system to rush to the heart and surrounding blood vessels. However, instead of having a healing effect, this can cause further harm and increase the risk of future heart attacks.
The clinical trial at Addenbrookes Hospital in Cambridge showed that the drug aldesleukin stopped this harmful immune activity. Using doses 1000 times lower than those used in cancer treatment, the team found it helped to calm inflammation and increase the anti-inflammatory properties of cells in the immune system.
February: Virtual Reality technology could help to repair hearts
Science fiction became reality in February when we learnt about immersive Virtual Reality (VR) technology, being developed at Evelina London Children’s Hospital, that could improve procedures for people with congenital heart disease.

Every day in the UK around 13 babies are diagnosed with congenital heart disease and some children will need one or more procedures to help their hearts function normally.
The VR technology brings together scans routinely used to plan these types of procedures to create a three-dimensional, beating digital double of the heart. The researchers think this will allow doctors to plan and practice these complex procedures using the virtual heart, before they get to the operating table.
They believe its use could also go beyond congenital heart disease and help plan any procedure that aims to repair a structural problem within the heart, such as valve surgery in an adult patient.
March: NHS roll-out of 'superhuman' 20 second AI heart tool begins
Artificial intelligence is without doubt fuelling a new era of medicine. Back in the Spring, our researchers announced that their new 20 second AI tool to detect heart disease in record speed was starting it’s roll-out in the NHS at University College London Hospital, Barts Heart Centre at St Bartholomew’s Hospital and Royal Free Hospital.
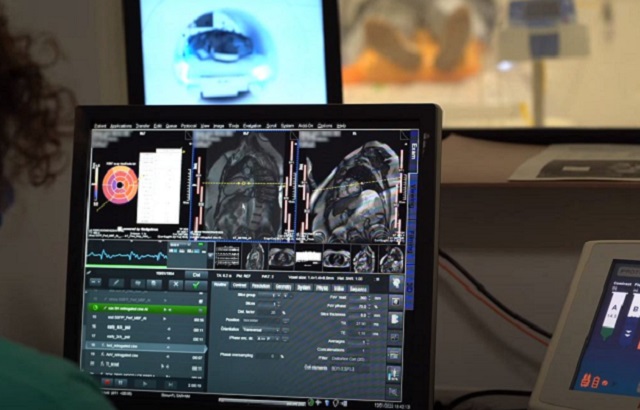
The AI can free-up valuable time of healthcare professionals – saving around 3,000 clinician days every year – so their attention can be directed to seeing more patients on NHS waiting lists, which will ultimately help with the backlog in vital heart care. It also gives patients and doctors more confidence in the MRI results so that they can make better decisions about a person’s treatment and possible surgeries.
Fast forward nine months, and their technology is now being used in Leicester, Leeds, as well as Minnesota and Milan! All-in-all, they are now analysing an estimated 1500 patients per month using the AI.
April: Number of people with stroke-inducing heart condition at all-time high
In April, our researchers unveiled data that found the number of people living with atrial fibrillation (AF) has increased by 72 per cent in England over the last two decades, now outstripping the number of people diagnosed with the four most common types of cancer.
Using anonymised GP and hospital data from 3.4 million people, they found the increase was regardless of sex and age, and largely due to an ageing and more unhealthy population. It also highlighted an unequal picture and that health inequity exists in AF.
This ‘blueprint’ of AF emphasises the need for more targeted prevention strategies and new innovations to equip doctors to better detect the condition early so people can benefit from anti-clotting drugs and other life-saving treatment.
May: Antibodies to unlock secrets of cholesterol
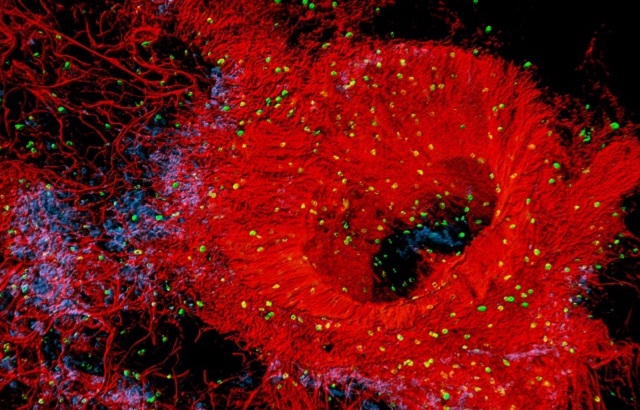
May brought news of a new way to understand and target fatty plaques in arteries called atherosclerosis, a common cause of heart attacks and strokes.
Researchers at the National Heart and Lung Institute, Imperial College London have created an antibody that can bind to the cholesterol molecules that make up these fatty plaques soon after they’ve been deposited in the artery wall.
While the research is still at an early stage, the team say it can help scientists to understand more about how these plaques develop. Eventually, it could also help doctors spot plaques in their patients’ arteries at an earlier stage, allowing people to make lifestyle changes and begin treatments that can slow their progression.
June: Injectable gel could help to heal damaged hearts
In June, the British Cardiovascular Society conference was held in person for the first time since 2019, bringing together hundreds of doctors and scientists to share the latest developments in heart and circulatory diseases research.

At the conference, researchers we’ve funded at the University of Manchester revealed that they have developed an injectable gel that could improve treatments that aim repair damage caused by heart attacks. They showed that the gel could support the development and growth of new heart tissue and encourage blood vessels to grow into that tissue, and that the gel could be safely injected into the beating heart.
While it’s still early days, this research is an important step towards treatments to repair damaged hearts and reduce the risk of heart failure.
July: £30m for scientists to rewrite DNA to cure killer heart diseases
July saw the biggest research moment in our 60-year history as we announced CureHeart as the winner of our £30m Big Beat Challenge.
The mission of CureHeart is to develop the first cures for inherited heart muscle conditions by rewriting DNA using pioneering and ultra-precise gene therapy that could edit or silence faulty genes that cause the deadly conditions.
Inherited heart muscle conditions can curse families for generations. Around one in 250 people worldwide are affected by these genetic cardiomyopathies, with a 50:50 risk they will pass their faulty genes on to each of their children. In many cases, multiple members of the same family will develop heart failure, need a heart transplant, or are lost to sudden cardiac death at a young age.
This global award presents a once-in-a-generation opportunity to relieve families of all these constant worries.
August: Statins aren’t the cause of muscle pain in most people who report symptoms
In August, thousands of doctors and scientists from around the world gathered in Barcelona for the European Society of Cardiology Congress. One of the biggest developments from the conference found that statins are not the cause of muscle pain in over 90 per cent of people who experience symptoms.
Statins are one of the most prescribed medicines in the UK, but side effects, particularly muscle weakness or pain, are reported by many people who take them. The researchers analysed data from 23 clinical trials, including information from almost 155,000 people, to find out once and for all whether statins cause muscle pain.
Similar numbers of people in the statin and placebo groups reported muscle symptoms. The team found that for every 1000 people taking a moderate intensity statin, the treatment would cause 11 (generally mild) episodes of muscle pain or weakness. This means that the benefits of taking statins to prevent heart attacks and strokes greatly outweigh the risk of experiencing muscle symptoms.
September: Protein discovery could provide heart attack lifeline
Every five minutes someone is admitted to hospital with a heart attack in the UK. When someone has a heart attack, the small vessels that supply the heart with oxygen-rich blood become blocked. When this happens, the heart muscle cells can die, and this can lead to heart failure.

But researchers at King’s College London have discovered three heart protective proteins, using new ‘search engine’ technology, that could one day be given to heart attack patients in the back of an ambulance to halt damage to the heart. This could lead to the first treatment of its kind.
More tests need to be done, but they hope the first human clinical trials will take place in the next two years.
October: Runners take to London streets to raise money for regenerative medicine
We were the TCS London Marathon charity of the year in 2022. The marathon on Sunday 4 October saw around 800 BHF runners take to the streets of London to raise money for lifesaving research into regenerative medicine, a cutting-edge field that has the power to unlock a cure for heart failure.

One of those runners was Professor Sanjay Sinha. When he’s not training for a marathon, Professor Sinha splits his time between treating patients and leading ground-breaking research to develop new treatments for damaged hearts.
Professor Sinha is creating a Heart Healing Patch, which is made of stem cells that have been triggered to develop into heart tissue. The result is a patch of heart tissue that contracts in a coordinated way, just like the heart muscle does when it beats. His is one of the projects that will be supported by the money raised through the London Marathon.
November: Simple 60-minute iron treatment can help avoid heart failure hospital admissions
Nearly one million people in the UK are living with heart failure. Up to half of these people also have low levels of iron in their blood, and this has been linked to worse symptoms, lower quality of life, and greater risk of hospitalisation and death.
But now, results from a clinical trial of over 1,000 people have shown that a simple, 60-minute iron infusion every one to two years could be beneficial for people with heart failure and low iron levels.
The results showed that iron infusions reduced the risk of being admitted due to heart failure and dying from a heart related cause, compared to usual care. The team hope their findings will lead to heart failure guidelines being updated to recommend patients’ iron levels are regularly monitored and topped up if they’re found to be low.
December: Stem cell plasters to stop children needing repeated heart surgeries
We ended the year with some festive cheer as we shared the news that we’ve awarded BHF Professor Massimo Caputo £750,000 to develop ‘stem cell plasters’ that could revolutionise the way surgeons treat children living with congenital heart disease, so they don’t need as many open-heart operations.

Currently, for many of these children, surgeons can perform open-heart surgery to temporarily repair the problem, but the materials used for the patches or replacement heart valves are not completely biological and cannot grow with the baby. This means they need multiple surgeries throughout their life.
The stem cell plasters are designed to be sewn into the area of the child’s heart that needs repairing during surgery. They could offer a solution that means their heart is mended once and forever in a single operation, preventing children like Louie from facing a future of repeated surgeries and giving them the gift of a happier and healthier life.


