

A drug developed by researchers at UCL can normalise blood vessel growth inside cancerous tumours and enable more effective delivery of targeted cancer treatments, according to research we’ve part funded published today.
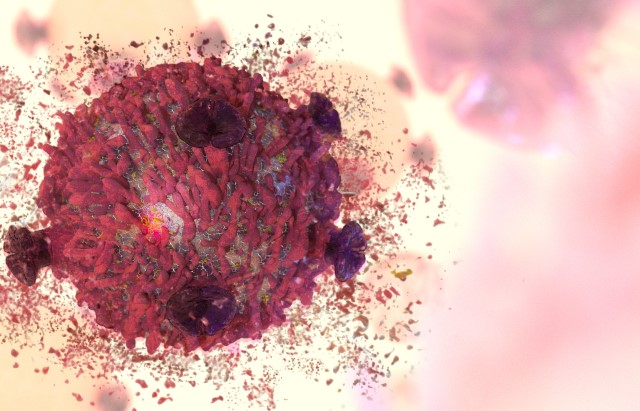
Disorganised blood vessel formation is a common feature in many conditions, including cancer. This affects the amount of oxygen that tumours receive, potentially making them more aggressive. It can also impact on the delivery of treatments designed to target and kill cancer as less of it is able to travel to the tissue affected.
In this study researchers investigated whether inhibiting the activity of LRG1, a protein produced in many tumorous tissues, could allow blood vessels in tumours to grow more normally. When mice with tumours were treated with the drug developed by the UCL team - an antibody that can bind to and block the activity of the LRG1 protein - it led to improved blood flow and reduced tumour growth rates.
Improving existing treatments
Some of the mice also received other cancer therapies in addition to the antibody drug, to mimic the types of treatment courses seen in humans. When the drug was combined with chemotherapy or immunotherapy (a type of treatment that helps your immune system fight cancer) the researchers saw an increase in number of immune cells within the tumour and greater tumour cell killing activity compared to treatment with the antibody drug alone.
The researchers say that the drug has the potential to improve outcomes in patients who respond poorly to current standard of care for cancers, including those of the breast, colon, bladder, prostate, and lung.
They have now developed a human version of the drug, which was originally developed around 10 years ago as a potential treatment for eye diseases, and this is ready to move into clinical trials in patients with cancer and eye disease
Potential for better results
Professor Stephen Moss, Norman Ashton Professor of Biomedical Research at the UCL Institute of Ophthalmology and co-lead of this research, said: “Although counterintuitive, finding a way to normalise cancerous tumour blood vessels has become a clinical objective, but identifying an effective therapeutic tool has proven elusive.
“Our results provide direct evidence that blocking the LRG1 protein, which is produced at high levels in tumours, normalises the vasculature and enhances the current sub-optimal effectiveness of immunotherapies, including checkpoint inhibition and CAR-T cell therapy, in solid cancers.
“This opens up the potential to achieve a far better result in many cancer patients who respond poorly to current standard of care.”
This research was also supported by funding from the Wellcome Trust and the Medical Research Council.


