“I’m so stressed” is a phrase we hear all the time. What is stress? And what does it mean for our health? In this series, we will examine some of the different types of stress our mind and body can experience. In part one we learnt how psychological stress can cause inflammation. In part two, we look at mechanical stress: the physical power of blood roaring round our heart and blood vessels all day, every day.

Part 2: Mechanical stress - under pressure
Our heart beats over 100,000 times a day, and every beat forces eight pints of blood around enough vessels to circle the globe. Twice.
Our blood vessels undergo an immense amount of mechanical stress across our lifetime. The walls of our vessels stretch and relax and constrict to accommodate changes in blood pressure, but what if that flexibility fails? If blood vessels stiffen this can lead to rising blood pressure and ultimately damage to the vessel or even the heart. If blood vessels lose their elasticity they can develop aneurysms - pockets that bulge out of the blood vessel’s normal shape and can break or ‘rupture’, leading to internal bleeding.
The largest blood vessel in our body
One such example is the abdominal aorta - the largest blood vessel in what we commonly call the ‘belly’. Aneurysms in this blood vessel can be detected but if they rupture, they are almost always fatal. The only treatment is major surgery which comes with its own risks. Professor Matt Bown at the University of Leicester is tracking thousands of men with aortic abdominal aneurysms in the hope that we can predict which aneurysms will grow quickest and be the most likely to rupture. The goal of this study is to highlight those that should be monitored most frequently, and to decide who needs urgent surgery. Detecting the aneurysms most likely to burst could save thousands of lives each year.

A vital support system
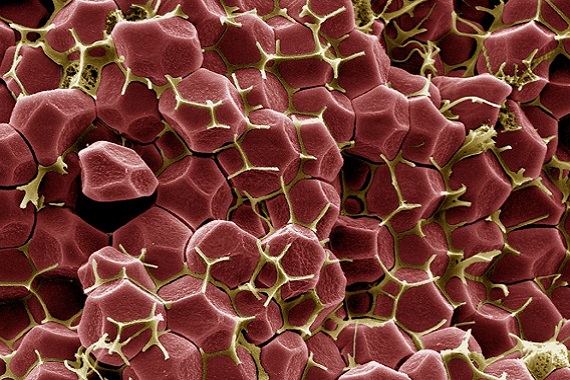
A major part of the structure of blood vessels and organs is a framework called the extracellular matrix, or ECM . It consists of strengthening and anchoring proteins and helps give surrounding cells structural support.
When an aneurysm begins to form, the ECM in that area of the blood vessel is degraded. This damage is either not repaired, or not repaired properly, creating a weakness in the blood vessel wall that makes a rupture more likely. Professor Manuel Mayr at King’s College London is studying the molecules of the ECM in healthy aorta samples, and samples from people with aneurysms. He hopes that by comparing the two he will discover the reason why the ECM changes as an aneurysm develops.
Our pumping machines
Our blood vessels are under pressure because of the blood being pumped around them. But what about the stress on the organ that does the pumping? Our hearts beat constantly throughout our lives, but if the heart is weakened by disease, the stress of constant activity or exercise can take its toll.
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a condition made progressively worse by the heart beating – just by being alive. Heart muscle cells stretch to pump and are held together with microscopic hooks called desmosomes. These anchor the cells to each other while allowing them to move. In ARVC, the ‘hooks’ fail to do their job well enough, and the heart muscle cells start to die leaving gaps between them. These gaps are filled with a fatty scar which not only does not beat, but also doesn’t conduct the electrical rhythm of the heart. This scar means the rest of the heart must work harder, which puts even more stress on the rest of the muscle. Over time, people with ARVC develop heart failure and can have a potentially fatal cardiac arrest.


In ARVC, heart cells pull apart from each other, leading to heart failure and even death
A faulty gene
Dr Vinoj George is trying to understand why some people’s ARVC is much worse than others. A faulty gene in someone’s DNA is associated with severe ARVC symptoms. Dr George is growing cells with this mutation to understand how this leads to the more severe cases. This could help us predict who is at most risk from ARVC, which causes 2-5% of young adult deaths.
The heart is a powerful engine, capable of pushing blood around the many thousands of miles of blood vessels in our body. That power, however, needs to be supported by healthy blood vessels if we are to avoid aneurysms. The mechanical stress our hearts and blood vessels generate and adapt to is incredible, but monitoring it is the safest way of ensuring the machine of the heart continues to help us.
Find out more about blood pressure
More BHF Research
Ever wondered which animal has the most complex heart? Or how what you drink can affect your health? How about if you can die from a broken heart?
Our brightest and best life saving research is brought to you each week.