

Eating a large meal could help detect early signs of metabolic conditions such as type 2 diabetes, according to new research we've part-funded, published in the journal Cell Reports.
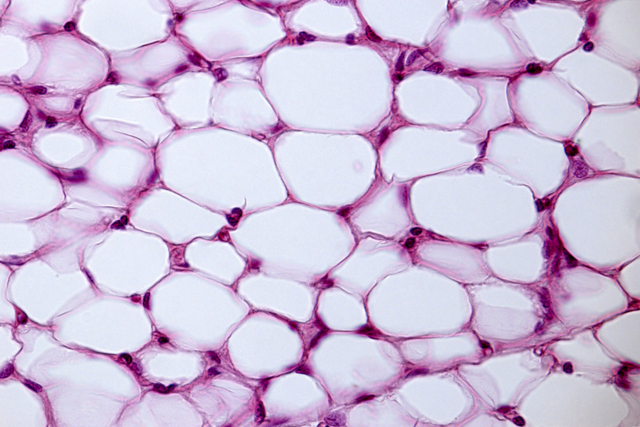
A team of researchers, led by Dr Samuel Virtue and Professor Toni Vidal-Puig of the Cambridge University Metabolic Research Laboratories and the Medical Research Council’s (MRC) Metabolic Diseases Unit, have made the observation whilst studying a gene called PPARy2. This gene controls the formation and function of fat tissue, which stores energy in the form of fat.
Researchers found that in mice that lack PPARy2, lipids - a form of free fat - were not sufficiently stored in fat tissue and were redirected to other organs, which is an early sign of metabolic disease and diabetes.
Although the young mice without PPARy2 looked ‘healthy’, they went on to develop insulin resistance (the process that underlies early diabetes) as they got older.
The glucose tolerance test (GTT) is a diagnostic test used routinely to detect diabetes. A glucose drink is taken after a period of fasting and the test measures how well the body’s cells are able to absorb glucose.
Signs of metabolic disease
When the team performed the GTT on the mice without PPARy2, the results were similar to normal mice. But when they replaced the glucose in the GTT with a large, fatty meal – equivalent to eating a Christmas dinner – signs of metabolic disease emerged, including 10 times the levels of insulin found in normal mice given the same fatty meal, increased blood glucose and increased blood fatty acids.
The researchers believe this is because PPARy2 is especially important in clearing free fats from the blood quickly after a high fat meal by storing them inside fat tissue. In mice without PPARy2, the fat tissue was overwhelmed by the high fat meal and the lipids built up in the blood or were redirected to other organs, eventually leading to insulin resistance as the mice aged.
Together with Professor José Manuel Fernández-Real, of the University of Girona, the team also demonstrated that PPARγ2 levels in humans are lower in obese individuals, demonstrating that their findings could also be relevant to humans. The study was jointly funded by the British Heart Foundation (BHF), MRC and Wellcome.
Fascinating new insights
Dr Lucie Duluc, our Research Advisor, said: “Over a quarter of adults in the UK are obese, putting them at a higher risk of developing diabetes and heart and circulatory conditions.
“This study provides fascinating new insights about the link between obesity and metabolic disease. One possible implication of the findings is that, in some metabolic disorders, it may be beneficial to eat small amounts of food more regularly rather than eating three larger meals a day. But more research is needed to make sure that these findings are applicable to humans.
“This research was only been made possible by the fantastic generosity of the public and their support to drive forward our mission to beat heartbreak forever.”
Better targeting of interventions
Professor Toni Vidal-Puig added: “With obesity levels on the rise, it is increasingly important to understand how obesity leads to metabolic diseases like diabetes.
“Overall, this study could help detect individuals with metabolic disease earlier than existing tests and allow better targeting of lifestyle and pharmacological interventions.
“Our research suggests that it may be easier to detect some individuals with early stage metabolic disease by testing them with a large meal, rather than using the traditional test of giving glucose after fasting. The results may also suggest that some individuals with early signs of metabolic disease could change their eating habits for several small meals rather than one large meal, so their fat tissue is never over-challenged.”


