What’s most exciting in
angina research right now?
Angina is a symptom experienced
when the blood vessels that supply the heart, the coronary arteries, narrow
and not enough blood gets to the
heart muscle. Most people have a type
called stable angina where
the narrowing of arteries happens
slowly over time.
Doctors previously focused on
opening the arteries of people with
stable angina in order to prevent heart
attacks from happening.
Now we are placing more emphasis
on people’s symptoms.
As a doctor and researcher, it’s rewarding to help people get back to what they enjoy.
When you speak
to people with angina, over a third will
tell you it seriously affects their quality
of life.
Because of the chest pain and
breathlessness they experience with
angina, they are no longer able to pick
up their grandchildren, or run for the
bus, for example.
Giving people with angina the right
medication or procedure lets them get
back to what they enjoy.
I’ve had patients tell me they’ve been
able to get back to playing in a band
because they can now lift their double
bass, or even that they completed
the National Three Peaks Climbing
Challenge after having the right
treatment. As a doctor and researcher,
that’s very rewarding.
How will research change the
way angina is treated?
I think the biggest difference is that
in 20- or 30-years’ time treatment will
be more personalised.
At the moment,
treatment for stable angina tends to be
one-size-fits-all, with most people put
on the same pathway.
Clinical guidance tells us to try
medicines first. Then, if that does not
work, they are offered a procedure
called angioplasty and stenting, where
a small tube called a stent is used to
reopen the arteries.
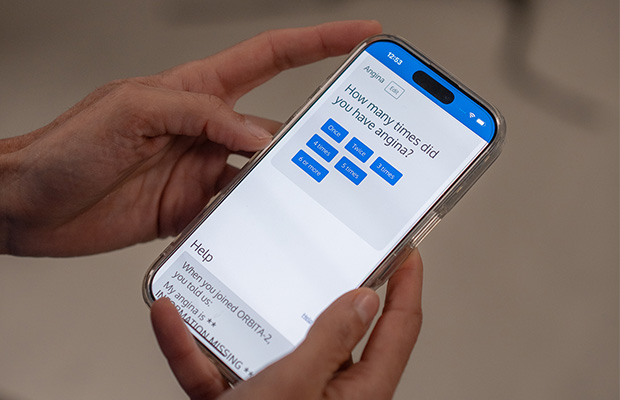
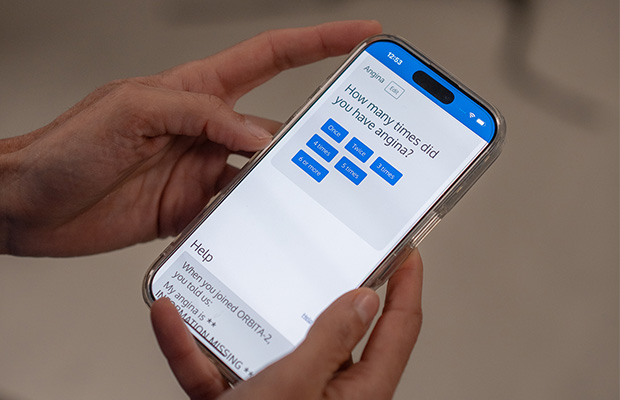
But through trials
I’ve conducted, called ORBITA and
ORBITA-2, it seems some people would
benefit from being offered a stent first.
This is particularly true of those
who experience pain in the middle of
the chest when they exert themselves,
which goes away when they rest.
I’d like to get to the point where the number of people still living with angina symptoms disappears.
We’ve also learned that not
everyone feels better with stenting.
Somewhere between 30 to 60 per
cent of people still feel symptoms after having a successful procedure.
So BHF
is now funding my work to find out how
we can target stenting to the people
who will experience the most benefit.
I am looking at the symptoms people
experience, what imaging technology
tells us about the narrowing of their
arteries, how these and other factors
are connected, and how they could be
used to predict who stenting will help.
I’d like to get to the point where the
number of people who are still living
with angina symptoms, despite having
multiple different treatments, is far
smaller, and maybe even disappears.
Why is it important for BHF to
fund research like this?
This is not the kind of research that
the medical industry would fund.
This is because my research has found
that expensive treatments are not
always as useful as we might think.
Also, it might not happen in other
countries, where clinical research is
not so closely linked to the healthcare
system, as it is in the UK.
Independent charities like BHF
recognise the importance of research
that investigates questions that matter
to patients.
Thanks to BHF funding, science like this has the potential to shape best practice across the world.
What happens if anti-anginal
medicines and stenting fail?
Some people with coronary heart
disease have treatment, including
medicines, stenting or a coronary artery
bypass, to open their arteries but they
still experience chest pain.
We call this refractory angina. It can
really affect people’s lives as they have
no other options for treatment.
In one of our trials, ORBITA COSMIC,
we tested the use of a new device
called a coronary sinus reducer.
In
regular stenting a stent is used to
widen the narrowed artery supplying
the heart. By contrast, the hourglass-shaped coronary sinus reducer is used
to narrow the heart muscle’s main vein.
This helps blood flow to areas of the
heart muscle not getting enough blood. Research may help this to become a
regular treatment option in the future.
Want to get fit and healthy?
Sign up to our fortnightly Heart Matters newsletter to receive healthy recipes, new activity ideas, and expert tips for managing your health. Joining is free and takes 2 minutes.
I’d like to sign-up
Microvascular angina is
another growing area for research.
Most medicines have been
developed to treat narrowing in the
main arteries that supply the heart.
They do not target the problems in the
very smallest of arteries which happen
with microvascular angina.
Now there are trials taking place,
including one funded by BHF, to test
out the coronary sinus reducer in
people with microvascular angina.
Other researchers are using new
imaging technologies to better
understand what is happening in these
micro vessels. Others are looking at the
biological processes happening in the
body in microvascular disease. With
better understanding, we’ll be able to
develop new treatments.
How do we prevent angina from developing?
I'm working with the medical journal The Lancet on a commission on exactly this issue: How do we get to the point where coronary heart disease stops being a very common disease and it becomes very rare or even disappears?
A big part of the answer is to help people reduce high blood pressure and cholesterol levels and control diabetes, to prevent these risk factors leading to the coronary heart disease, which is one of the main causes of angina.
In recent years we’ve seen the development of exciting new cholesterol-lowering drugs and ones that target diabetes. Also, guidelines are changing so that we’ll be targeting patients to lower their blood pressure and cholesterol levels at an earlier stage.

What made you interested in researching angina?
I've always been interested in clinical trials and how the results can affect how we actually treat people. I wanted to study a disease that was common and to design clinical trials that would have an impact on the greatest number of people.
Over a million people in the UK live with angina and it can create a significant burden on their ability to live their lives.
Also, across the world, over 500,000 stenting procedures are done every year to treat angina. This has a big economic burden but importantly it carries some short and long term risks for patients, so we want to make sure we are only performing this procedure for the people who actually stand to benefit from it.
Meet the expert
Dr Rasha Al-Lamee is an interventional cardiology consultant at Imperial College Healthcare NHS Trust in London. Alongside seeing patients, she is funded by British Heart Foundation (BHF) as a research fellow at Imperial College London.
What to read next...