Digital transformation within a clinical pathway
Introduction
As a frontline clinician, you may find yourself thinking "there must be a better way." Digital is often a go-to, to address inefficiencies. It may be that you feel you can improve:
- Systems
- Processes
- Patient experience
Or you could be looking to reduce administration and free up time on patient care.
Technology isn’t a panacea, but it can help with these challenges – and more.
We’ve created this resource to support frontline healthcare staff considering digital transformation who feel unsure how to proceed.
How can digital transform the patient pathway?
Some applications of technology within healthcare include:
- Collation and analysis of patient data to inform clinical decision-making
- Increasing data-sharing/data flow among clinical teams
- Remote patient monitoring
- Automation of routine tasks to free-up time
- More accurate patient information to create tailored support
- Reaching people who may not otherwise engage in healthcare
- Supporting patients to engage in their healthcare more actively
Professor Tim Chico, Personal Monitoring Data Thematic Lead and Associate Director at the BHF Data Science Centre, said, "Digital is another way of talking about information flow. How do you know what information you need? How do you collect it? Who needs access? One of the biggest transformations I've seen is the shift from paper printouts for blood tests. Often, paper printouts were in physical locations and often lost or overlooked."
Dr Raj Thakkar, Primary Care Cardiology lead, Oxford AHSN, said, "If you can close the gap between patient and clinician, you'll bring healthcare to the patient."
"By focussing on fixing specific and defined problems, technology solutions can reduce workload and improve both access and outcomes for patients and the wider NHS. By way of example, evidence suggests that systems can significantly improve engagement between patient and clinician by delivering healthcare directly to the patient rather than expecting a patient to travel to a facility physically."
Improving a clinical pathway using digital technology
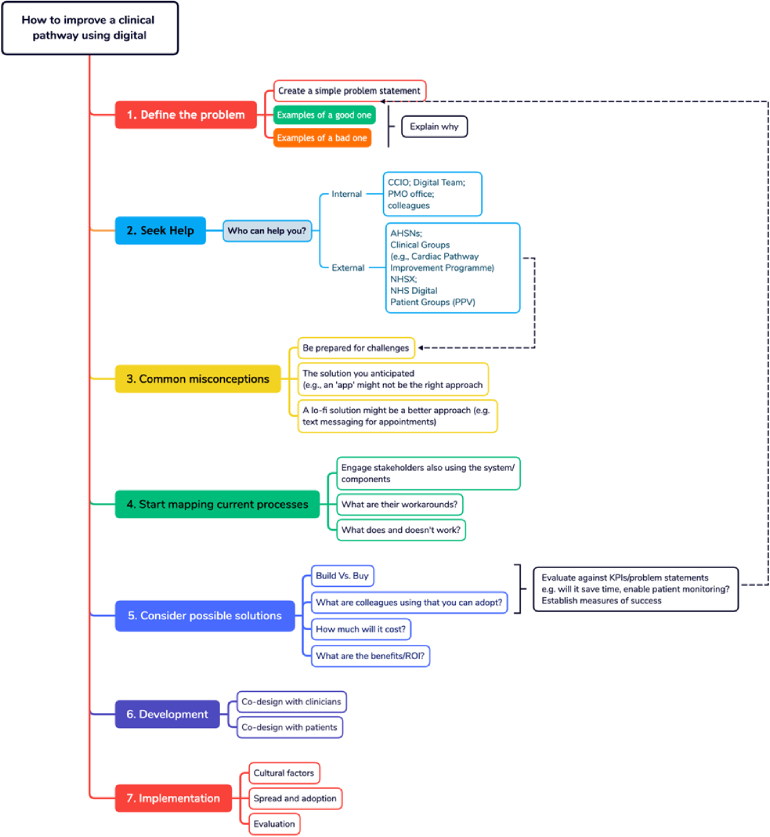
This flowchart illustrates the seven steps you can take to improve your clinical pathway through the implementation of digital technology.
Download a copy of the flowchart in PDF format using the button below.
Overview
It’s tempting to rush for a solution. Yet, experts agree it is fundamental to start with the problem you are trying to solve.
Adrian Byrne, Chief Information Officer at University Hospital Southampton NHS Foundation Trust, said, "Many digital solutions exist, which are trying to find a problem. It’s the wrong way round."
Instead, a problem statement should define a specification of requirements.
Debashish Das is a Consultant Cardiologist at Barts Hospital NHS Trust and gives an example of a 'problem' around consultation times. Appointments are 30 minutes long, regardless of patient need. Yet, some cases are more complex than others.
So, consultants may spend more time with stable patients than they need.
How would you define this as a problem statement? We’ve provided a ‘good’ and a ‘poor’ example to help you draft your statement.
Good example
"How do we tailor appointment times for cardiology patients by need? The aim is to spend more time with complex cases while maintaining routine check-ups for all."
Poor example
"Can we build an app that lets patients self-monitor their condition at home? By sharing data with us, we can assess how much time they’ll need in the clinic and only see patients who need us."
Let’s deconstruct them.
In the ‘good’ example, we define the problem and desired outcomes as an open question.
The ‘poor’ example assumes that:
- The solution demands an app. Digital may form part of the solution, but it may not require an app.
- The clinician will build the app rather than buy one.
- The answer is for patients to self-monitor.
- Patients will record and share data.
- It will be possible to estimate how much clinic time each patient requires.
- Clinicians will only see patients with acute needs.
There are three things you’ll need to begin your digital transformation journey. First, you’ll need commitment. The second is time. Finally, you’ll need help.
You’ll need support from experts in digital transformation.
So, who are they – and how do you find them?
We’ve separated the potential roles into internal and external resources.
Internal support
You’ll need technical support. You won’t find what you are looking for through your IT Helpdesk.
If your organisation has one, the Chief Information Officer (CIO) is your first point of call.
Another potential route is through the Project Management Office (PMO).
It’s also wise to engage chief clinical information officers and hospital consultants. Both can lend credibility to your business case.
When it comes to buying solutions, you’ll need to engage procurement teams, too.
We’ll explain where to draw on their support as we explore how to map existing processes, evaluate possible solutions, and develop and implement them.
External support
You may also need to look externally. Some areas to explore include:
Academic Health Science Networks (AHSNs, England only): England's 15 AHSNs operate as the key innovation arm of the NHS.
Clinical Groups: Join clinical groups for support.
Communities of Practice: A community of practice (CoP) is a group of people who share:
- a common concern
- a set of problems
- an interest in a topic
They come together to fulfil individual and group goals. For example, the Health Innovation Network hosts groups across south London. Groups share innovation and ideas.
Conferences: Attending conferences is an excellent way to discover what others are doing.
NHS Digital: Designs, develops and operates national IT and data services. Services support clinicians at work, support patient care, and use data to improve treatment.
NHSX: The transformation directorate of the NHS (England-specific but includes valuable resources for all).
Before embarking on a digital transformation journey, it’s worth addressing common misconceptions. Doing so will ensure that you and your digital colleagues have a shared view and lexicon to develop possible solutions.
- Technology will solve everything: digital is likely to form a part of the solution, but technology won’t solve everything. You should also consider the impact of introducing technology, such as the need for change management and leadership.
- Buy solutions at conferences: It’s easy to be wowed by high-tech solutions at conferences. Yet, the best solutions may not solve your specific problem. Likewise, it may not be compatible with your existing technology. Share ideas with digital colleagues but don’t buy solutions without due diligence. Conferences are full of people selling innovative solutions promising quick implementation. You may be unaware of the work it will incur from digital teams.
- All solutions will be hi-tech: Sometimes solutions are lo-fi. Improving routine procedures can save time and money. For example, you could replace paper-based appointment letters with email and text. "Technology can't solve everything, and it is essential to assure yourself that what you purchase will solve your specific problem and not create any new ones," said Dr Raj Thakkar, GP and Primary Care Cardiology lead Oxford Academic Health Science Network. "Some tasks that we perform in healthcare are relatively low value. And, if we can automate these lower-value processes, clinicians can be released to focus on higher-value tasks such as managing complex co-morbidities or end-of-life care," he added.
Before you make changes in your system, map your existing processes. Create a process map. You can seek support from within your organisation. It could be the digital team, Project Management Office (PMO) or transformation team. Process mapping is a simple exercise in your toolkit of improvement methods. It helps a team know where to start improving for the biggest impact for patients and staff.1
A map of the patient’s journey is a crucial starting point for any improvement project, large or small. You should tailor it to suit your organisation or individual style2. Process mapping will clarify where to make improvements. It may also throw up inefficiencies or barriers you haven’t identified yet. Process mapping will help you to3:
- Set clear and focused goals
- Evaluate whether a change is a genuine improvement
- Clarify and document existing processes
- Bring together a multi-disciplinary team around a common problem
- Consider the potential unintended consequences of a solution
Adrian Byrne, CIO of University Hospital Southampton (UHS), said, "Process mapping is a great place to start, but not everyone will have the skills. We [the digital team] would engage in a bit of time to support with process mapping if people need help articulating a story."
He added, "initially, you are just looking for a document that says, ‘these are my problems.’ If they can do process mapping and diagrams, then fantastic."
The NHS Institute for Innovation and Improvement has a guide to Improvement Leaders’ Guide Process mapping, analysis and redesign. The guide explains the benefits of process mapping, who to involve in designing a process map and how to create a basic map.
1 Improvement Leaders’ Guide Process mapping, analysis and redesign. NHS Institute for Innovation and Improvement (2017).
2 Improvement Leaders’ Guide Process mapping, analysis and redesign. NHS Institute for Innovation and Improvement (2017).
3 List summarised from Improvement Leaders’ Guide Process mapping, analysis and redesign. NHS Institute for Innovation and Improvement (2017).
Involve stakeholders, including patients and clinicians
Creating a process map is a stage where you may wish to involve patients and clinicians. Both are the key users of the system and will know where the problems lie.
Involving patients doesn’t mean you must make every single change they identify. Your digital team will help you prioritise. It will create a minimal viable product (MVP).
After release, you can make incremental improvements.
Once you’ve established the root cause of the problem, you can consider possible solutions. Some common decisions you may face during the process include the following:
- Build vs Buy – should you build your solution?
- Existing solutions – Are colleagues using systems that may benefit you?
- Costs, risks and benefits – how much does it cost versus the potential return on investment?
- KPIs – what does success look like?
Build vs Buy
Should you build a solution or buy one? It’s a common dilemma. Generally, there is no need to create something bespoke if a solution exists.
However, the downside of buying something is that you won’t own it and have less control over the features.
"We always prefer to buy the bulk of functionality off-the-shelf rather than, you know, getting bespoke software written for everything that we do," said Adrian Byrne, CIO of University Hospital Southampton.
So, how do you know?
Return to the problem statement and your process map. What is the problem you are trying to solve? If it’s a simple one where an off-the-shelf or existing solution is available, your digital department will inform you (see existing solutions).
Existing solutions
The challenge might be a lack of communication between hospital or organisation colleagues. Your digital team will know if it has existing solutions that you could use, such as Microsoft Teams. Or you might be looking to invite people for appointments using text messaging. Similarly, there may be a solution in place.
"Sometimes it's obvious. It’s a messaging requirement, and we have strategic platforms for messaging," says Adrian Byrne, CIO for University Hospital Southampton.
For example, you may have seen a solution that fits the bill at a conference. If so, it’s essential you share details with your digital team, which can evaluate compatibility with existing systems and the level of support it would need.
Where a solution isn’t immediately apparent, it doesn’t mean one isn’t available. Your digital team may offer to put the problem into the market and see if a solution fits the bill. You could also reach out to colleagues with a shared problem and see how they’ve addressed it.
Conferences can be an excellent place to seek solutions, but you’ll need to evaluate whether they meet your needs.
Costs, risks and benefits
Costs will depend on the solution. Evaluate any possible costs against return on investment. For example, your organisation may be willing to invest more if a solution frees up consultants’ time and is scalable.
Build an evaluation of ROI into process mapping.
Moving into deployment and development, consider engaging audiences who’ll use the revamped pathway. That includes clinicians and patients if changes will affect them.
Involve clinicians in the development
Clinicians, said Debashish Das, Consultant Cardiologist at Barts Hospital NHS Trust, can be forgotten in the development process. "I've seen many lovely patient-facing tools but have put no thought into clinician workflow. Does it save the clinician time? It must work for the clinician, too."
Involve patients in changes to the pathway
Of course, it must also work for patients.
"You've got to find a good reason not to involve patients (unless you’re solving a technical issue). If a problem affects patients, it's mission-critical to involve patients and their carers in developing any new approach. Otherwise, you'll run a very high risk of missing an essential consideration and ultimately failing in your change programme," said Dr Raj Thakkar, Primary Care Cardiology Lead for Oxford AHSN.
"The one thing I could hopefully suggest to people thinking about any form of digital transformation is to get a patient and public group together. Do it from the earliest opportunity and work with them to co-design," agreed Professor Tim Chico, Personal Monitoring Data Thematic Lead and Associate Director at the BHF Data Science Centre.
Chico stresses the importance of creating a diverse group representing the patients using it. Professor Chico’s tips are:
- Consider where you hold the meetings – community settings are more accessible.
- Think about the time of day you hold meetings.
- Is there funding available? Can you attract more people by offering to pay costs (e.g., travel and childcare)?
Adrian Byrne, CIO of University Hospital Southampton, offers an important caveat. He advised you do not build for perfection or a complete version of the specification. The 80:20 rule applies, and you will hit the law of diminishing returns as you invest more time in the last 20% than in the first 80%. Deliver a minimum viable product if at all possible. "If you aim for 100%, I guarantee you’ll focus most effort on the last 10%."
Likewise, there could be technology that can solve a problem that users are not aware of. You need to allow the digital team to propose solutions not just listen to what users want, or think they want.
"We go through an iterative process in design until you get to the eventual product. Even when you deliver version 1.0 live, you're probably two versions away from the product they will eventually be happy with," said Byrne.
Transformation means change, so it’s vital to consider change management within your project. How will you change the way people work? Consider engaging digital champions to support your transformation programme. How will you engage patients to pilot the first version of your product, and what support will they need to ensure success?
Compliance
There are other considerations, too—notably, digital compliance. To get a digital health product into the NHS, it should comply with the Digital Technology Assessment Criteria (DTAC). Likewise, if you’re buying in or procuring digital products, check that they are DTAC compliant.
As the NHS transform website says:
The DTAC is designed to be used by healthcare organisations to assess suppliers at the point of procurement or as part of a due diligence process to make sure digital technologies meet our minimum baseline standards. For developers, it sets out what is expected for entry into the NHS and social care.4
Similarly, you need to consider whether any devices patients use meet specifications. Data from consumer devices such as activity trackers and smartwatches aren’t classed as medical devices. "Doctors are split 50/50 as to whether they will look at your tracker data," said Professor Tim Chico, Personal Monitoring Data Thematic Lead and Associate Director at the BHF Data Science Centre. "The data can be useful, but it is not a medically approved device," he added.
Some devices are approved for certain functions but not others. It’s an essential consideration if you plan to use these devices as part of your digital transformation journey.
The UK Government offers guidance on regulating medical devices in the UK.
4 Source: Transform England
Results from our survey on Digital Health Technologies for Heart Failure
We conducted a survey of people involved in the use, implementation, and development of technologies used to help treat or care for people with heart failure in England. Take a look at the results, including in-depth information on the purpose of these technologies and how they are used.
How to transform a digital pathway
Expert Contributors
The BHF is very grateful to the following experts who contributed to this article:
Professor Tim Chico: Associate Director at the BHF Data Science Centre and Personal Monitoring Data Thematic Lead
Dr Raj Thakkar: Primary Care Cardiology Lead, Oxford AHSN
Dr Debashish Das: Consultant Cardiologist, Barts Hospital NHS Trust
Mr Adrian Byrne: Chief Information Officer, University Hospital Southampton NHS Foundation Trust

