The journey to a cure
CureHeart’s ambition is to reach early clinical trials in 5 years. See our journey to trialling a cure for inherited heart muscle diseases.
What's on this page:
Key Milestones
A project of this scope and scale has different elements and approaches which will progress in parallel - just like a river, which has streams joining it at different points.
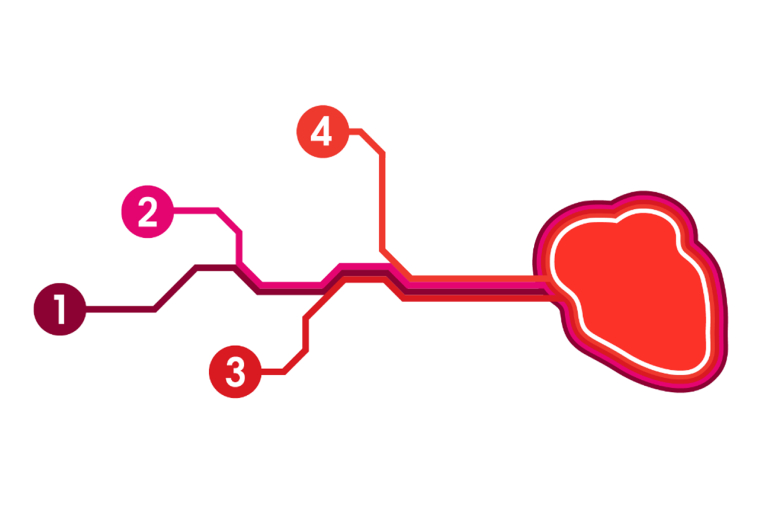
Here are some of the workstreams the CureHeart team will be working on over the next few years. It is hoped that the discoveries and outputs from these will result in at least one of the most promising therapies entering early-stage testing in people living with inherited heart muscle diseases in four to five years’ time.
There are also answers to some of the questions you may have about the project, which can be found lower down the page.
Key Workstreams
1. Patient-facing work
Patients and their family members are central to the CureHeart project, and they are involved as research partners at every stage. Effective patient involvement from the outset and throughout the programme is essential for developing new and effective therapies.
Some of the ways in which patients will be involved include:
- Sharing their experience to help the team prioritise the biggest problems for patients
- Providing patient voices on attitudes to different types of treatment
- Helping the team understand the needs of patients, and what information is important to them
- Helping to recruit participants for trials, and deciding what represents a successful outcome from the patient perspective
Patients also sit on two groups related to CureHeart: the British Heart Foundation (BHF) Oversight Panel, and the Ethics Advisory Group. A patient, and patient representative Joel Rose of Cardiomyopathy UK, also sit on a Scientific Steering Committee. This makes sure patient voices are always part of discussions about the direction of the project as it develops.
Another important focus of this workstream will be to identify and prioritise those groups of patients that are most in need of new genetic treatments.
Combining expertise across a range of areas, including genetic research and advanced heart imaging, the CureHeart team will build a comprehensive picture of disease burden. This information will be used to guide the team and help them decide which groups of patients to target first.
2. Develop genetic therapies
Complex tools are needed for genetic therapies and these tools must be designed specifically for each faulty gene the team wish to treat. Designing the most effective tools is a challenging process which takes time and substantial testing to ensure the therapies are safe and effective.
Two different approaches are being explored.
Antisense silencing is already being used to treat certain other conditions. It doesn’t change the faulty DNA code but stops it producing faulty proteins. Repeated treatments could stop symptoms and disease from developing or progressing.
Gene editing, on the other hand, does alter the DNA in the cells of the heart. It could be used to correct mistakes in a faulty gene, switch a faulty gene off altogether, or boost production from a healthy copy of a gene to compensate for lack of production by a faulty one.
It is crucial to make sure these gene edits act precisely on the mistake being targeted within heart muscle cells, and do not affect other cells of the body. The team will rigorously test editing tools in the laboratory ahead of any trials.
Advancing antisense silencing and/or gene editing therapies to early clinical trials would be a major success in the battle against inherited heart muscle diseases.
3. Target therapies to the site of disease
Many delivery strategies are being developed in parallel, to directly target treatments to the diseased heart muscle. Different delivery strategies will be required depending on the genetic therapy being used, and the team will pair each therapy with the most suitable delivery technique.
Both therapies could be delivered by a simple injection, like many other treatments we already receive. While our knowledge of the best delivery methods for antisense silencing therapies is more advanced, less is currently known about how to effectively deliver gene editing therapies to the heart muscle. The team will consider:
- The best packaging to get therapies to the heart
- Which cells to target, and how many of them need to receive editing to halt symptoms
- The effectiveness and potential side-effects of different delivery approaches
4. Give therapies the greatest chance of success
New genetic therapies could be transformative for some groups of patients living with inherited heart muscle diseases. For those living with more established or advanced cardiomyopathy, new treatments could be less effective because of years of accumulated injury to the heart.
This could make disease more difficult to reverse and could even prevent new therapies from reaching heart muscle cells. To ensure that any new therapy has the best chance of being effective, the team are testing approaches to reduce or reverse existing damage and scarring in the heart to improve the effectiveness of the new genetic therapies.
The power of industry partners
At the right time, pharmaceutical companies will become involved to bring a therapy to the clinic. This is because they have the resources and facilities to manufacture and test the therapies developed to ensure they meet the highest standards required to administer to patients.
What will success look like?
The goal of CureHeart is to develop cures for inherited heart muscle diseases.
Along the way, the team will innovate to develop new gene silencing and editing tools and better packaging systems to deliver those tools to exactly where they are needed most.
By the end of the research programme (late 2027), we hope to be ready to start a first trial in patients.

