
Leicestershire man is 100th recruit in landmark heart failure clinical trial



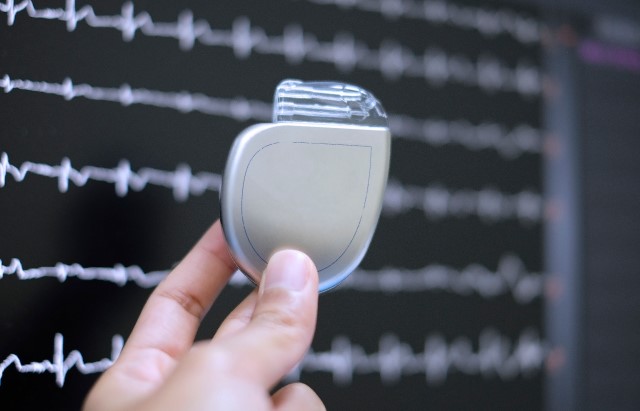
Peter Dyde, 68 a retired businessman from Hinckley had an implantable cardioverter defibrillator (ICD) fitted in July. The ICD will now monitor Peter’s heart rhythm and, if it detects any abnormalities, will spring into action to shock his heart back into a normal rhythm and stop a cardiac arrest.
Influence guidelines
The trial aims to recruit 1,250 people with non-ischaemic cardiomyopathy – which can cause heart failure – across 35 UK hospitals over the next three years.
The team leading the study hopes that the results will influence clinical guidelines in the UK and around the world, helping to improve quality of life and survival for people with heart failure.
In heart failure, the heart can’t pump as well as it should meaning too little blood and oxygen reaches the rest of the body. This can cause symptoms such as breathlessness, tiredness and swollen ankles.
It’s estimated that more than one million people in the UK have heart failure, and a further 200,000 people are newly diagnosed every year. Around one third of heart failure patients have non-ischaemic cardiomyopathy, which can lead to abnormal heart rhythms.
Scar tissue
People with heart failure are often fitted with an ICD, which acts as an insurance policy against a cardiac arrest. Currently patients are assessed to see how well their heart is pumping and determine whether they receive an ICD.
But Dr Andrew Flett, a consultant cardiologist at University Hospital Southampton who is leading the BRITISH trial, believes that current guidelines may mean that people are being fitted with an ICD who will never benefit.
The study will trial an alternative approach, instead looking at the amount of scar tissue in a patient’s heart. Scarring can develop because of a number of conditions, including heart attacks, heart valve diseases and toxicity due to cancer chemotherapy. It is thought that this scar tissue interrupts the circuits that carry electrical impulses through the heart and cause it to beat.
Driving progress
Patients with non-ischaemic cardiomyopathy whose heart scans show evidence of scar tissue will be invited to take part in the trial. Half of the patients will be randomly assigned to be fitted with an ICD.
The other half will receive an implantable loop recorder, a small monitor fitted under the skin that records the heart rhythm but does not shock the heart. This will allow the researchers to review any abnormal rhythms these patients may experience.
The researchers will follow participants for three years after they’ve had their ICD or loop recorder fitted to determine whether having an ICD improves survival.
Professor Bryan Williams, our Chief Scientific and Medical Officer, said: “Thanks to our incredible supporters, the BHF has a proud history of funding pioneering research that has saved and improved the lives of countless patients.
“This trial has the potential to influence treatment for heart failure patients around the world. But studies like this are only possible thanks to people like Peter, whose generosity helps to drive progress in treatment and care for the benefit of heart patients long into the future.”
 Peter knows all too well the devastation that heart problems can cause. In June 2018 he and his wife Kim lost their eldest daughter Charlotte aged just 34 to cardiomyopathy – a condition which affects the heart muscle and can lead to cardiac arrest.
Peter knows all too well the devastation that heart problems can cause. In June 2018 he and his wife Kim lost their eldest daughter Charlotte aged just 34 to cardiomyopathy – a condition which affects the heart muscle and can lead to cardiac arrest.
Peter said: “You wonder why something like that should happen to you. But I’ve learnt since that we’re part of such a big club, there are so many people affected by heart conditions. It wouldn’t help me to stay in a dark place in life. We can’t help what happened to our family, but we can try and help make things better for others in future.”
“When my consultant mentioned the BRITISH trial I just said ‘sign me up’. The way I look at it is that by taking part I could help to save someone else’s loved one, or stop another family going through the same as us. When you think about it like that, there's nothing really to decide.”
“The doctors have been brilliant, they’re helping me so much. By taking part in this trial I’m able to give back to them too.”

