

January: Figuring out how our blood vessels are made

We kicked off the year by funding some exciting research into the role of genes in congenital heart defects. Researchers are looking into how genes are expressed in a tissue called the pharyngeal endoderm during development. This tissue is close to where the large vessels of the heart are formed.
They hope that by identifying which genes are important in blood vessel development they can identify how they interact with one another and discover how they can cause defects in the heart. This research could pave the way for future screening for these genes and lead to prevention and treatment for heart defects.February: Takotsubo cardiomyopathy – trying to understand a mysterious disease
In February, we gave researchers at the University of Aberdeen £215,000 to launch a landmark Scottish study on Takotsubo Syndrome.
This mysterious condition, described by researchers as a “neglected area of cardiology”, presents like a heart attack, and is often triggered by severe emotional distress, such as the death of a loved one. As a result, when it was first discovered, it was also referred to as “broken heart syndrome”. However, researchers now believe it can be caused by several different factors, including intense physical trauma, or in some cases no trauma at all.
By examining data from all recorded cases of the condition in Scotland since 2010, scientists hope to discover exactly what happens to people when they have a sudden episode of Takotsubo.
March: AI tech to help predict heart attacks
Using artificial intelligence to predict a heart attack may sound like science fiction, but technology funded by us that can do just that was approved by the EU in March. The first-of-its-kind technology, CaRi-Heart® uses routine heart scans already performed in clinical practice to detect ‘invisible’ risk in people with possible heart disease.
Each year in the UK hundreds of thousands of people go to hospital with chest pain. A coronary CT angiogram (CCTA) scan is the first-line test for patients with angina and is used to check for any narrowed or blocked segments in blood vessels that supply the heart. However, 75 per cent of these scans do not show significant narrowing of the arteries and so people are sent home without treatment, yet some of them will have a heart attack at some point in the future. Until now, there has been no way for doctors to detect all the underlying red flags that could lead to a future heart attack.
April: The importance of lowering blood pressure revealed

In April researchers found that lowering blood pressure is even more beneficial than previously thought. Blood pressure medication can prevent serious heart conditions such as stroke, heart attack and heart failure even in adults whose blood pressure in the healthy range.
Researchers looked at the data of 344,716 participants from 48 trials over four years. Analysis revealed that reducing your blood pressure by 5mmHg can reduce your risk of cardiovascular disease by 10 per cent and your risk of death as a result by 5 per cent, even if your blood pressure is healthy. Even more reason to know your numbers by getting your blood pressure checked regularly.
May: Helping hearts to beat stronger
A staggering 920,000 people in the UK are living with heart failure, and there is no cure. After a heart attack the heart muscle can become damaged making the heart weaker and less able to pump blood effectively around the body. There is an unmet need for drugs that make the heart beat stronger but many drugs that do so are deemed unsafe.
Switching off heart a protein could be the answer. Scientists found that high levels of a protein called MARK4 were present after a heart attack. After a heart attack, in the heart muscle cells of mice without MARK4, the speed of contraction increased by 42 per cent and the speed of relaxation increased by 47 per cent, compared to muscle cells from mice with the MARK4 protein. They were also close to functioning at the same level as healthy heart muscle cells, showing the power of lowering levels of MARK4.
Scientists hope that a drug that switches off MARK4 could offer a promising new way to improve recovery and help the heart to pump blood more efficiently in patients with heart failure.
June: Injectable microspheres to help repair damaged hearts
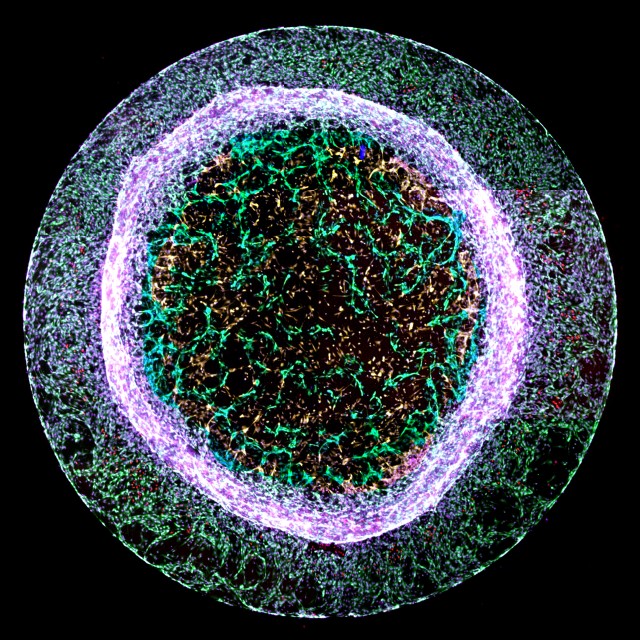
June saw the British Cardiovascular Society conference go virtual. Scientists we fund presented injectable microspheres as an innovative way to deliver human stem cell-derived heart cells directly into the heart.
Researchers have been trying to use stem cells to repair the damage to the heart seen in heart failure for many years. However, these cells often don’t remain in the heart in a healthy state for long enough to provide a sustained benefit.
Now, the team have grown human stem cell-derived heart cells on tiny microspheres, each only one quarter of a millimetre wide. The cells attach to the microsphere, make connections with each other and are able to beat just like the heart cells found in the heart for up to 40 days in a dish. It is hoped that this will provide a viable therapy for those suffering with heart failure in the next 10 years.July: Energetic clues could help people with diabetes recover after a heart attack
Researchers discovered that diabetic hearts lose energy during heart attacks. High fat levels in the hearts of people with type 2 diabetes might make their cells ‘immune’ to the important roles that fats have in regulating cells’ energy consumption.
During a heart attack, the hearts of rats with type 2 diabetes use up their energy supplies more quickly than those without the condition. This leaves their hearts with less energy – a strong predictor of worse outcomes after heart attack.
The findings might help to explain why people with diabetes are more likely to develop heart failure after a heart attack than people without diabetes. They also reveal potential targets for treatments that could reverse these effects and help diabetic hearts to recover after a heart attack.August: Beautiful science!
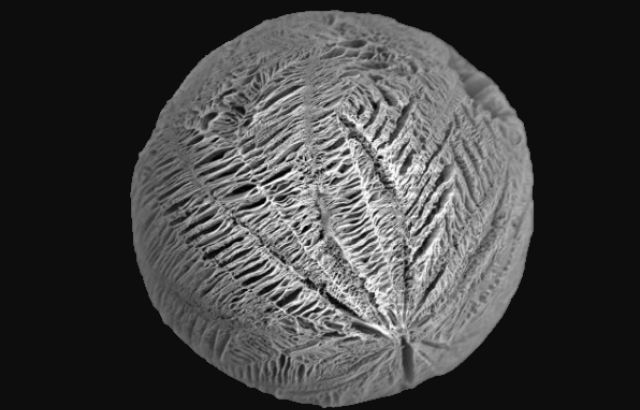
In August we announced the winner of our annual national science image competition ‘Reflections of Research’. This year’s winner was Dr Elisa Avolio from the University of Bristol with an incredible image that appears at first glance to resemble a luminous jelly fish, but in reality, shows new blood vessel-like structures (pictured in green in the centre) sprouting from a 3D gel.
Her research is looking at ways to encourage new blood vessels to grow in the heart to restore blood supply to areas of the heart that have been damaged. This knowledge could help treat patients after a heart attack in the future.September: Hope for incurable vascular dementia
A drug, already on the market for the treatment of high blood pressure, could present a potential new drug for incurable vascular dementia. High blood pressure is known to increase a person’s risk of developing vascular dementia, but how this causes the small vessels of the brain to narrow and restrict vital blood supply to parts of the brain was unknown.
Now researchers have found that amlodipine, a drug commonly prescribed to treat high blood pressure, could halt this devastating disease in its early stages. Mice who were treated with the drug were found to have better blood flow than those not treated with the drug. They also identified a protein in the small vessels called Kir2.1 shows deceased activity in mice with high blood pressure.
Researchers say that this protein could also be targeted by other drugs in the future, presenting a potential additional way to help fight the disease.October: A new heart transplant technique for children
October saw researchers funded by us at Great Ormand Street Hospital pioneer a new technique that makes heart transplants possible for more children in need. Now double the number of children will be able to receive a heart transplant, giving them hope for longer and happier life.

In the past 20 years, doctors have been able to perform more heart transplants on children by developing a technique which allows hearts from donors with a different tissue type from the recipient to be transplanted. However, this technique involves the child’s blood being removed, and their circulation ‘washed’ out’ by blood matching the donor heart. This requires a lot of blood and so is limited to children under 4 years old.
Now, the team have found a way to use a special blood filtering device - called an immunoadsorption column – during the transplant operation to reduce the amount of blood needed and allow children as old as 8 to receive the transplant they desperately need.November: Clot busting drug for stroke
In November researchers found a new clot busting drug that could improve stroke treatment. This drug was found to break down blood clots in the brains of mice who are resistant to current medication.
A stroke happens when the blood supply to the brain is cut off. The most common cause of this is a blood clot in one of the major arteries that supply the brain, meaning that the brain is starved of oxygen.
Alteplase is currently used to treat patients who have had a stroke. However, this does not work in 50 per cent of patients, who have a clot rich in a protein that plays a crucial role in clot formation called Von Willebrand Factor. This new drug could offer a potential treatment for patients who have a blood clot rich in this factor.December: Better protection during surgery
We finished up the year by awarding £570,000 to a clinical trial that could help improve the recovery of children who undergo life-saving heart surgery. The study will compare two ways of protecting the hearts of children during surgery to repair congenital heart defects.
During open heart surgery, a fluid called cardioplegia is commonly used to stop the heart beating so that the surgeon can repair it safely. While this technique is safe, damage to the heart muscle may be caused when blood flow returns to the heart, which can affect the child’s recovery.
This study will compare the type of cardioplegia currently in use with a new type called del Nido cardioplegia, which is commonly used in the US, in the hope of identifying which type leads to better patient outcomes.

None of this ground-breaking research would be possible without you. With your continued support, we will be able to fund even more cutting-edge research into the world’s biggest killers throughout 2022 and beyond.
Learn more about our research successes


