


What is cholesterol?
Cholesterol is a fatty substance in our blood. It is naturally produced by our liver, and everyone has it because we need to stay healthy — every cell in our body uses it.
Cholesterol is carried around the body in our blood streams by proteins (the building blocks of our cells). When cholesterol and proteins are combined, they are called lipoproteins.
Why is high cholesterol bad?
There are several types of lipoproteins, but they can generally be divided into two main types, you may have heard them referred to as ‘good’ and ‘bad’ cholesterol, also known as HDL and LDL cholesterol respectively.
High-density lipoproteins (HDL) are known as ‘good’ cholesterol because it gets rid of ‘bad’ cholesterol from our blood vessels. It takes the cholesterol that we don’t need back to the liver where it is broken down and removed from your body, which lowers our risk of heart and circulatory diseases.
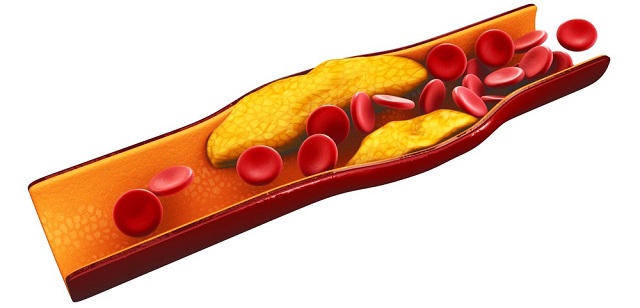
Low density lipoproteins (LDL) deliver cholesterol from the liver to cells around our bodies. This is known as ‘bad’ cholesterol because, if there is too much cholesterol circulating in our bodies, it can stick to the walls of our blood vessels. This can clog up the blood vessels, causing them to become stiff and narrow which can lead to a heart attack or stroke.
There are several types of lipoproteins, but they can generally be divided into two main types: ‘Good’ HDL cholesterol and ‘bad’ LDL cholesterol.
If you have been told you have a high total cholesterol level, you have too much ‘bad’ cholesterol in your bloodstream which means you are more likely to have a heart attack or stroke. But a high level of ‘good’ (HDL) cholesterol can help keep that ‘bad’ (non-HDL) cholesterol in check.
What should my cholesterol level be?
When people talk about keeping their cholesterol down, they usually mean their total cholesterol level- the levels of ‘good’ HDL cholesterol, ‘bad’ non-HDL cholesterol and levels of triglycerides (fatty substances that can contribute to the blockage of blood vessels).
There is no specific target cholesterol level. Instead, your doctor will look at your overall risk of developing heart and circulatory disease. This assessment will include things like whether you smoke or have high blood pressure.
For a healthy heart, the aim is to have a low non-HDL (bad) level and a high HDL (good) level.
How can I reduce my cholesterol levels?
Anyone can get high cholesterol, and it can be caused by many different things. Some things you can control, like lifestyle habits, and others you can’t.
Things that cause high cholesterol you can control:
- - Eating a lot of saturated fat
- - Smoking
- - Not being active enough
- - Having too much body fat, especially around your middle
But there are also things that cause high cholesterol you can’t control, like getting older, your gender, and your genetic background — certain inherited conditions like Familial Hypercholesterolaemia cause high cholesterol that can’t be controlled by diet and lifestyle changes.
What are statins?
Cholesterol-lowering medicines such as statins are prescribed for people who are at greatest overall risk of heart and circulatory disease.
Statins are the most commonly prescribed medicines in the UK and they are used to lower the level of cholesterol in your blood. They work by inhibiting an enzyme in the liver called HMG-CoA reductase, which reduces the production of cholesterol in the liver and therefore leads to reduced cholesterol levels in the blood. There are different types of statins, but they all work in much the same way.
As there are lots of different types of statins, it’s about finding the one that works well for you, in a similar way to women finding a type of oral contraceptive pill that works best for them and their bodies. Lots of people don’t need a strong statin to reduce their cholesterol level. Your GP or cardiologist will help to find the right statin for you, depending on your medical history and the cholesterol level they think you should aim for.
If you’re sensitive to one statin, you might not be sensitive to another. If you have any questions about your statins, you should talk to your doctor being making any changes to your medication.
Do they work?
With all the conflicting headlines, it isn’t surprising that we can be confused about the effects of statins, but there is a lot of research that can inform our decisions. Large clinical research studies, involving many thousands of people, have shown that lowering bad cholesterol reduces your risk of heart disease — especially heart attacks.
How do statins prevent heart attacks and strokes?
In 1989, BHF Professor Stuart Cobbe led a trial which revealed that people with high cholesterol could reduce their risk of having a first-time heart attack by nearly a third by taking statins. This was followed by a study carried out by BHF Professor Sir Rory Collins 1994, which showed that even people with ‘normal’ cholesterol could lower their risk of future heart attack or stroke by taking statins.
Today, statins are the most commonly prescribed drug for those at risk of developing heart disease and are estimated to save thousands of lives each year in the UK. They act to reduce the likelihood of a heart attack or stroke, and their impact is most strongly seen in people most at risk, such as those who have already had a heart attack or stroke, but they are still effective at protecting those who haven’t yet suffered a heart attack or stroke.
But don’t they cause side effects?
Like all medicines, statins have potential side effects. Serious side effects are rare and can be reversed if you stop taking the statin. The most common are muscular aches and pains, but many people experience none at all.
A BHF-funded team at the University of Leeds has recently shed light on how statins can lead to muscle pain. They studied the effects of taking statins in rats and in samples of muscle taken from people being treated with statins. They identified that, in certain people, statin treatment can cause calcium ions to be released from certain parts of the skeletal muscle cell. This release of calcium can lead to the death of the muscle cells, starting the process of damage and statin myopathy.
Most interestingly they also found that, contrary to previous thinking, moderate exercise could help to benefit these people. Rats that undertook exercise while being treated with statins showed no obvious changes in their muscle.
Dr Sarah Calaghan, Associate Professor in Cardiac Physiology from the University of Leeds said:
“The idea that exercise makes statin side effects worse might be a misconception — what really matters is the intensity of exercise. We found that moderate exercise cancelled out the changes in muscle cells caused by statins. We know around 7 in 10 professional athletes can’t tolerate statins — and we know that intense endurance exercise has profound effects on the gatekeeper proteins targeted by statins. The added effect of statins could push muscles over the edge, leading to symptoms.
“The good news is, after twenty years of searching, we finally have an explanation for statin-associated muscle pain, along with a possible solution. If you weren’t convinced to exercise already, here’s another reason.”
So there may be steps we can take to reduce side-effects, should they happen, but we still don’t completely understand why certain people are more susceptible than others.
Who will get statin side effects?
A BHF team at the University of Oxford, led by Dr James Sheppard, aims to understand more about who is more likely to have side-effects when taking statins. To do this, they will compare a number of previous clinical trials testing statins (a ‘network meta-analysis’). This will produce a ranked list of each type of statin and dose levels based on their effectiveness and side-effects. Dr Sheppard will also compare this information to the GP health records of people who took statins (and those who didn’t), between 1998 and 2019 to look for evidence of new muscle symptoms, new-onset diabetes, liver injury, kidney dysfunction, haemorrhagic stroke and eye diseases that could be attributed as side effects of taking statins.
Their goal is to create risk calculators that doctors can use to estimate a person’s risk of side effects from statins. This will allow doctors and their patients to make a shared decision about whether to start, stop, or continue statin treatment.
Are there any alternatives to statins?
There are alternative drugs that work to lower levels of cholesterol in our blood, but in a different way to statins. PCSK9 is a protein which helps to stop the liver removing cholesterol from our systems. Therefore, more PCSK9 protein leads to more cholesterol in our circulation. Recently, drugs that limit PCSK9 — known as PCSK9 inhibitors — have been shown to reduce blood cholesterol in certain groups of people.
In 2016, the National Institute for Health Care and Excellence (NICE) recommended two PCSK9 inhibitors be used for people with conditions called primary hypercholesterolaemia or mixed dyslipidaemia, who can’t tolerate statins or who have reached the maximum dose but still require treatment for high cholesterol.
“Creating new treatments which use this approach could prove life-saving for patients with high cholesterol and those who can’t tolerate statins.” — Professor Sir Nilesh Samani, BHF Medical Director
What to remember
There are many actions you can take that can help to lower your cholesterol levels, including taking statins if your doctor prescribes them. If you have questions about your health, why you may have been prescribed statins, or what effects they may have, speak to your GP.
Read Statins: fact or fiction?
More BHF Research
Ever wondered which animal has the most complex heart? Or how what you drink can affect your health? How about if you can die from a broken heart?
Our brightest and best life saving research is brought to you each week.



