Familial hypercholesterolaemia
Some people are born with familial hypercholesterolaemia (FH), a genetic condition where your liver can’t process cholesterol properly.

Familial hypercholesterolaemia (FH) is caused by an inherited genetic defect, resulting in abnormally high total and LDL cholesterol levels in the blood. Early detection and treatment with lipid-lowering drugs can increase life expectancy to near normal.
Around 1 in 250 of the population1 have FH (260,000 people in the UK) but most remain undiagnosed. High cholesterol levels develop from childhood and result in a higher risk of early heart disease.
Studies have shown that the risk of developing coronary heart disease is up to 13 times higher in people with untreated FH.
However, early detection and treatment with lipid-lowering drugs can increase life expectancy to near normal.
Cascade testing of first-degree relatives of those with suspected FH is highly cost effective. High levels of undetected FH in the UK and associated morbidity and mortality mean that adopting cascade testing should yield substantial quality-of-life and survival gains in addition to reducing costs from avoidable CHD treatment.
The BHF commissioned a paper published in the European Heart Journal that concluded that testing is highly cost effective and would prevent thousands of premature heart attacks.
This approach provides the evidence to develop a FH cascade testing service across regional healthcare systems, bringing together primary and specialist secondary care services to more effectively and efficiently identify and treat undiagnosed FH and reduce premature heart attacks and deaths.
NICE has emphasised the need for “a nationwide, family-based, follow-up system” to enable comprehensive identification of people affected by FH.
Supporting the implementation of FH cascade services across the UK has brought to light a variety of local and system level barriers and enablers that are contributing to the current variation in access to services across the country.
FH cascade services test, diagnose and manage patients and relatives with inherited high cholesterol.
In the 1990s, Professor Steve Humphries made many important discoveries about the faulty genes that cause FH. His BHF-funded research led to the development of a blood test that shows whether someone has a fault in one of three key genes.
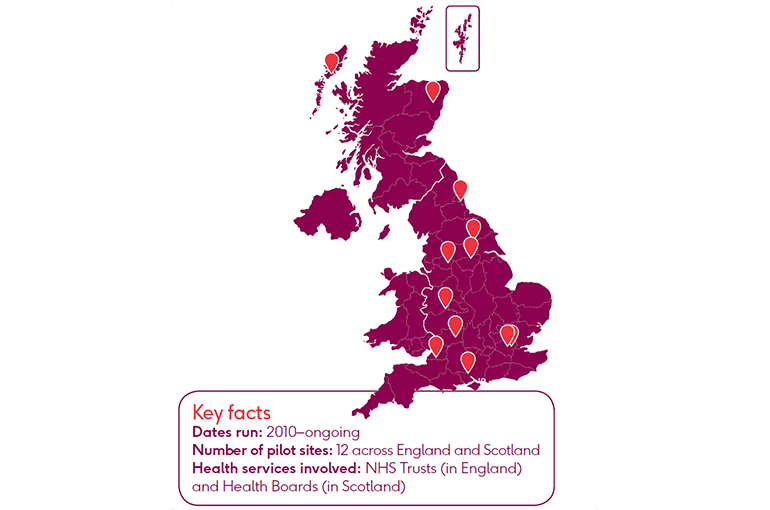
Over the past decade, the BHF has pioneered a cascade testing service to identify and treat first-degree relatives of people with FH in England and Scotland, following a successful scheme in Wales.
When cascade testing began in 2010, Wales had just 97 known FH patients. Since then, at least 2,616 previously undiagnosed case of FH have been identified across the UK as of June 2018.
We fund research into heart and circulatory disease and ensure discoveries from the lab bench make a difference at the patient’s bedside. FH is just one example of that work in action.
Step 1
GP refers patient with suspected FH to one of the lipid clinics, where family history is discussed.
Step 2
An assessment is made using the Simon Broome criteria and initial treatment begins to reduce cholesterol.
Step 3
The patient is referred to the clinic’s FH specialist nurse, who arranges a genetic test alongside blood cholesterol (LDL-C) concentration measurement.
If the patient tests gene-positive for FH, they are referred for family cascade testing, where immediate relatives are invited for testing and treatment. If any of them test positive, then their immediate family are also invited for testing.
Suzanne Sheppard is painfully aware of the devastation heart disease can cause.
Her father suffered a fatal heart attack in 1988 when he was 41 and she was just 15. His father had also died unusually young, due to a heart attack. This was the first clue that something wasn’t right. Suzanne’s cholesterol was twice normal levels. But no one could tell her why.
Thanks to the BHF’s part-funded pilot cascade testing programme in Wales, Suzanne finally found a reason for her high cholesterol: FH. With a single DNA test, one of the FH nurses identified that Suzanne had inherited a faulty gene which had caused her to have raised LDL cholesterol levels from birth. Her son, Cameron, has a 50/50 chance of inheriting the condition.
He will be tested when he is ten.
Cascade testing reduces the average age at which FH patients are diagnosed and treated. So we aren’t just waiting around for a heart attack to happen.
In 2008, the NICE clinical guideline 71 reported that diagnosing and treating people with FH and contacting their families through a systematic process of cascade testing provides one of the best opportunities for keeping patients healthy and out of hospital. The updated 2018 guideline has since called on GPs to search primary care records to find patients with signs of the condition. It also reiterated the importance of genetic testing to confirm a diagnosis – and for their family members to receive cascade testing.
In 2010, the BHF launched a pilot scheme, with an initial investment of £450,000, to provide a proactive interface between primary, secondary and tertiary care in Wales. Our funding paid for specialist clinical nurses for the first three years of the service.
The pilot was a partnership with NHS Wales, the Welsh Assembly Government, with support from HEART UK and the Genetic Alliance.
After the initial success of the Wales scheme, we extended the programme. In 2014, a further £1.5m was invested to continue identifying FH in England and Scotland. Across the 12 sites, FH nurses coordinated new service models, including primary or secondary care-led models and more nuanced dual-care models.
NICE estimates that if 50% of the predicted relatives of people with FH were diagnosed and treated, the NHS could save £1.7m per year on healthcare for heart disease by preventing cardiovascular events.3
In our FH programme, the estimated incremental cost effectiveness ratio (ICER) per relative tested was £5,806, far below the NICE threshold of £20,000–£30,000.
Our clinical summary booklet describes how improving services to identify, diagnose, risk stratify and optimally manage people with FH and their families can improve patient outcomes, and includes supporting evidence for implementation and replication.
Get this publication
To highlight the emerging issues in delivering FH services and inform senior decision makers in healthcare, we commissioned an independent report that gathers evidence from key stakeholders involved in delivering, planning and commissioning FH services.
In 2019, we published a review, Familial hypercholesterolaemia: Cascade testing in the UK today (PDF), which explores the issues and challenges of establishing an FH service and aims to help promote discussion about how to progress the FH agenda within the CVD community.
FH services differ across the UK, leading to unwarranted variation in patient care. The videos below showcase patient experiences of FH services in their area, ranging from a missed diagnosis (non-optimal pathway) to the best possible care (optimal pathway).
The FH Paediatric Register aims to allow monitoring of the safety and efficacy of current and new treatments and to provide anonymised data for valid research in the field.
The register is hosted by the Royal College of Physicians in collaboration with the Royal College of Paediatrics and Child Health, HEARTUK, the BHF and the British Inherited Metabolic Disease Group.
The following resources have been developed to:
Planning
NHS RightCare offers best practice guidance and case studies for a range of CVD conditions, including FH:
Lipid Clinics Map (Heart UK)
Heart UK publishes a map of lipid clinics across the UK.
FH register and audit
The Royal College of Physicians (RCP) hosts a FH register and audit to establish effectiveness of current therapies for children with FH. This includes a map of participating hospitals. The BHF has a representative on the UK FH Paediatric Register Steering Committee.
The RCP newsletter keeps clinicians who work with children with FH up to date with how many children are on the paediatric FH register, resources and analyses of the data collected. You can read the latest newsletter via the Paediatric Register website. The newsletter is accessible via the left-hand menu.
Poster resources
BHF-funded FH nurses have produced a series of conference posters [ZIP download], describing different aspects of FH services in their area.
1 Wald, D. et al (2016) Child–Parent Familial Hypercholesterolemia Screening in Primary Care. N Engl J Med 2016; 375:1628-1637. DOI: 10.1056/NEJMoa1602777
2 BHF (2015) Innovation in Practice
3 Heart UK. Saving lives, saving families. The health, social and economic advantages of detecting and treating familial hypercholesterolaemia (FH). 2012