The CVD Challenge in Northern Ireland
We have seen a significant reduction in premature deaths from cardiovascular disease (CVD) in Northern Ireland. However it's still a major cause of death and disability in the region.
Please note: This content was published in 2018 and is no longer being updated. The information on this page is for reference only.
Despite significant success in reducing premature mortality from cardiovascular disease (CVD), it remains a major cause of death and disability in Northern Ireland.
We look at eight reasons why tackling undiagnosed medical risk factors, improving quality of care and reducing variation can change millions of lives.
1. After 40 years of falling premature CVD deaths, progress has slowed
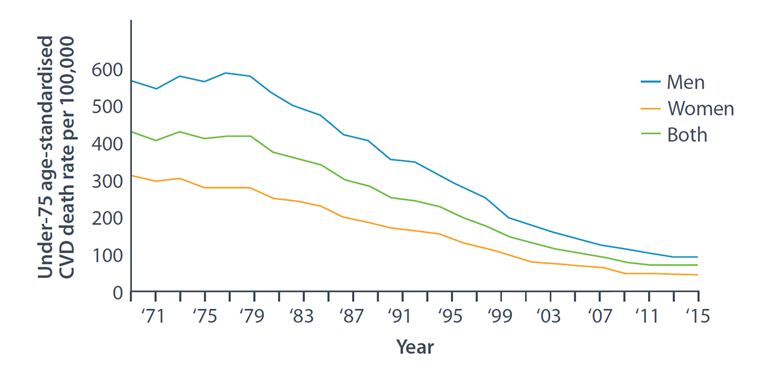
Data source: [1]
Around 19% of all premature deaths in Northern Ireland – 1,100 a year – are caused by CVD1
Today, cardiovascular disease (CVD) continues to affect the lives of thousands of people and is one of the largest causes of death and disability in Northern Ireland.
Premature CVD death rates in Northern Ireland have fallen 83% over the last 40 years1 largely thanks to BHF-funded research, advances in treating conditions like heart attack and stroke and the decline in smoking, as well as lifestyle changes.
But progress has slowed since 2011. The reasons are unclear. We must do more.
2. We are living longer, but with more long-term conditions
Data source: [2]
Our population is ageing. Growing life expectancy coupled with the ageing of the ‘baby boomer’ generation means the number of people aged over 65 is growing faster than those under 65.3
In Northern Ireland today, 225,000 people live with CVD;4 at least 16,500 of those have heart failure.5 CVD makes up a significant proportion of all long-term conditions (LTCs). Many other common LTCs also increase the risk of developing CVD.
What’s more, CVD risk increases with age: almost 8% of people in their 60s are diagnosed with coronary heart disease, for instance, and over a third will have hypertension,6 which increases the risk of other CVD conditions.
By 2030, the population in Northern Ireland aged 65-84 will rise by 37% and those over 85 by 76%.7
We must plan for the future.
3. CVD healthcare costs Northern Ireland hundreds of millions of pounds a year

Data source: [8]
The direct and indirect costs of CVD to the NHS in Northern Ireland and the wider economy are significant.
Each year, Northern Ireland spends an estimated £412m on CVD healthcare costs. The wider economic impact of these diseases is estimated at £600m.8
Meanwhile, the NHS in Northern Ireland needs to make efficiency savings of £1.9bn by 2020/21.9
We can bring down this cost.
4. You’re up to 30% more likely to die early from CVD depending on where you live

Data source: [10]
CVD risk factors such as smoking, physical inactivity and obesity are more common in deprived areas of Northern Ireland. These increase risk of hypertension, atrial fibrillation (AF) and high cholesterol.
So the most deprived people in our society shoulder the greatest burden of death and disability from CVD.
For instance, people living in the local authority with the highest level of average deprivation – Derry & Strabane – are 1.3 times more likely to die prematurely from CVD compared with people in Lisburn & Castlereagh, which has the lowest average deprivation in Northern Ireland.10
We must close this inequality gap.
5. We could perform better against other EU nations for premature CVD deaths
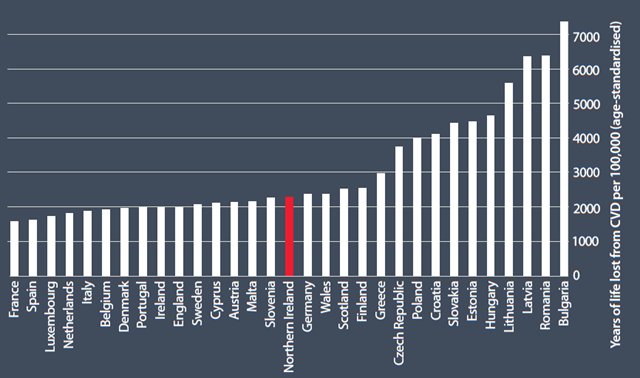
Data source: [11]
Despite decades of success bringing down the premature CVD death rate, Northern Ireland still ranks lower than 15 other EU nations – behind Slovenia, Cyprus and Malta.
Northern Ireland's premature CVD death rate is 45% more than France, which has the lowest rate among EU countries.
We can do better. Together, we can act to reduce this burden.
Millions of people have undetected medical risk factors that increase their chance of developing CVD. We can diagnose and treat them earlier.
Many with diagnosed risk factors receive sub-optimal treatment. We can improve care.
Patients experience varying standards of care and outcomes depending on where they live. We can innovate to improve patient outcomes.
6. Thousands could benefit from earlier risk factor detection and treatment
![]()
Data source: [12]
We know that hypertension is implicated in half of all strokes and heart attacks.12
People with AF are five times more likely to have a stroke.12
High cholesterol is common in the adult population. Raised cholesterol increases the risk of heart attack and stroke.12
However, we already have effective treatments available.
- Every 10mmHg drop in blood pressure reduces the risk of strokes and heart attacks by 20%.12
- Anticoagulation for AF prevents 66% of related strokes.12
- Every 1mmol/l fall in LDL cholesterol from statin treatment reduces yearly risk of heart attack and stroke by 25%.12
The problem is that significant regional variation in detection rate and treatment remains.
7. Better risk factor management could avoid thousands of CVD events
The missed opportunities

17% of adults with diagnosed hypertension (42,900 people) are not treated to guidelines

51% of adults with 10-year CVD risk above 20% (estimated at 66,900 people) are not treated with statins

10% of high-risk AF patients (2,600 people) are not anticoagulated
The potential
Over 3 years, optimally treating adults with diagnosed hypertension can avoid:
- 380 strokes
- 260 heart attacks
And optimally treating high-risk AF patients can avoid:
- 210 strokes
Data source: [13]
8. It’s time to think differently about CVD services
The BHF has piloted and evaluated models of care that can avoid hospital admissions, improve patient outcomes and save the NHS millions of pounds a year.
Now they need wider roll-out.
Atrial fibrillation
The challenge
Around 210 strokes in Northern Ireland could be avoided over three years[13] if everyone with AF was diagnosed and received appropriate anticoagulation therapy.
The solution
Arrhythmia Care Coordinators (ACCs) can help to enhance and optimise AF detection and management, reducing stroke incidence.
Find out more about the role of Arrhythmia Care Coordinators.
Familial hypercholesterolaemia (FH)
The challenge
The inheritable FH gene leads to abnormally high blood cholesterol levels, raising an otherwise healthy person’s risk of dying from a heart attack in their 20s, 30s or 40s.
The solution
Cascade testing first-degree relatives of people with FH can help identify and treat at-risk family members. A BHF pilot has so far found over 1,400 cases and offered treatment to lower CVD risk.
Learn more about our FH service.
Hypertension
A significant proportion of adults with hypertension remain undiagnosed. Of those who are, one in six are not treated to target. [5]
How can we do better?
The BHF and partners in primary care, public health and the third sector came together to produce a resource that highlights these problems and offers solutions.
Read our High blood pressure: how can we do better? resource.
References
1. BHF (2018) CVD Statistics Compendium 2018
2. Royal College of General Practitioners (2016) Responding to the needs of patients with multimorbidity: A vision for general practice
3. The King's Fund (2012) Demography: future trends
4. BHF (2017) estimate based on GP patient data and latest UK health surveys with CVD fieldwork
5. Department of Health Northern Ireland (2017) Quality and Outcomes Framework 2016/17
6. The Health Improvement Network (THIN) database (2017) version THIN1405
7. Office for National Statistics (2015) 2014-based National Population Projections
8. BHF analysis of European Heart Network (2017) European Cardiovascular Disease Statistics 2017 and Hospital Information Branch, Department of Health Northern Ireland 2014/15
9. Department of Health (2016) Systems, Not Structures - Changing Health and Social Care
10. BHF (2018) analysis of Office for National Statistics (2017) and Northern Ireland Statistics and Research Agency (2017) mortality data for 2014-16
11. Global Burden of Disease (2015)
12. NHS England (2016) The NHS RightCare Cardiovascular Disease Prevention Pathway – Dr Matt Kearney and Miles Freeman blog post
13. BHF analysis (2018) based on NHS England/Public Health England (2017) The Size of the Prize in Cardiovascular Disease (CVD) Prevention

