Stroke - TWIST
Should you treat people who wake up with a stroke with clot busting medicine?
The clinical question
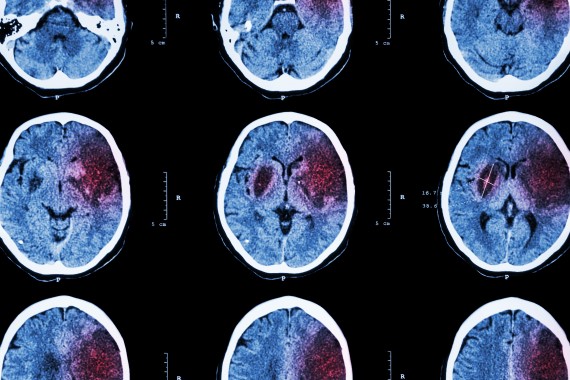
The usual treatment for a stroke caused by a blood clot in the brain (ischaemic stroke) is to give patients clot busting therapy - if the ‘clot buster’ drug can be given within 4.5 hours of the onset of symptoms (a crucial time window where the benefits of treatment have been shown to outweigh risks, such as bleeding). But what should doctors do if patients don’t know when they’ve had a stroke? This happens frequently in ‘wake-up stroke’, where people have a stroke while they are sleeping and then wake up with symptoms. It often isn’t known when exactly symptoms developed, and these patients are usually not offered clot busting therapy.
The results of recent trials have suggested that clot busting treatment might benefit people with wake-up stroke, specifically when specialised imaging scans can pin point that the stroke has probably taken place within 4.5 hours of waking, or that the part of the brain affected by the stroke is not irreversibly damaged. But the sophisticated type of imaging used in these clinical trials is not available to all patients.
The international Tenecteplase in Wake-up Ischaemic Stroke Trial (TWIST) was designed to find out if routine imaging with a simple CT scan (used in everyday practice) could identify patients with wake-up stroke who might benefit from clot busting therapy.
What did the study involve?
TWIST was an international trial led from Norway, which took place at 77 hospitals in 10 countries around the globe, including in Scandinavia, Finland, Estonia, Latvia, Lithuania, New Zealand, Switzerland and the United Kingdom. The British Heart Foundation funded the UK arm of the trial.
Between June 2017 and Sept 2021, 578 people with wake-up stroke were recruited into the trial, 165 of them in the UK.
People were screened for the trial if they had stroke symptoms and if the clot busting drug tenecteplase could be given to them within 4.5 hours of waking.
All patients then had a CT scan to see if they were eligible to enter the trial. They were excluded from participating in TWIST if the CT scan showed a bleed in the brain (where clot busting treatment is contraindicated), if the area of brain damaged by the stroke was very large, or if their symptoms were very severe – instances where it’s known that clot-busting treatment is unlikely to be beneficial, and therefore the risks of treatment outweigh the potential benefits.
Participants were then randomly assigned to be given either:
- The clot busting drug, tenecteplase, as an injection into a vein.
- Standard care with no clot busting therapy.
The CT scan was repeated after 24 hours to see if there was an improvement, and a clinical examination was performed after seven days or on discharge from hospital. At 90 days after entering the trial, members of the trial team telephoned participants to collect information on their functional outcome, which reflects the amount of disability caused by the stroke. For example, participants were asked if they could carry out usual daily activities, if they needed help with walking, or if they were bed bound. The team also asked about quality of life and tested memory and thinking ability.
What did the study show?
- The trial was disrupted by the COVID-19 pandemic and was stopped when 578 of the planned 600 patients had been recruited.
- Almost half of people given tenecteplase (45%) achieved an excellent functional outcome as did 38% in the control group. Treatment with tenecteplase did not significantly improve the amount of disability caused by the stroke compared with the control group when measured at 90 days.
- Bleeding into the brain causing symptoms (which is a potential side effect of tenecteplase) occurred in a similar small proportion of patients in both groups — 6 patients (2%) in the tenecteplase group versus 3 patients (1%) in the control group.
- Overall, the trial did not support giving tenecteplase to people with wake up stroke selected by performing a simple CT scan.
Why is the study important?
About 20–25% of stroke patients wake up with stroke symptoms and don’t know when their stroke happened. According to current guidelines, this large group of patients are excluded from receiving clot busting therapies. As there is no other specific drug treatment for stroke, trying to identify a subgroup of these patients who could benefit from clot busting treatment — the aim of the TWIST trial — is vitally important.
Unfortunately because of the COVID-19 pandemic, the TWIST trial investigators were unable to recruit the target number of participants and the study may therefore have been too small to detect any potential benefits offered by tenecteplase treatment.
A comparison of the treatment and control groups as part of the trial analysis showed that more patients in the control group than in the tenecteplase group were treated with thrombectomy — where the blood clot blocking the blood vessel in the brain is removed through a catheter (14% in the control group had thrombectomy vs 6% in the tenecteplase group). When a procedure like thrombectomy is performed to physically remove the clot, it is less likely that a clot busting drug will have a big effect and this difference between the groups could have affected the results of TWIST.
In light of these results, it remains uncertain whether tenecteplase is of benefit to people with wake up stroke.
Professor Thompson Robinson, Principal Investigator of the UK trial commented:
“The United Kingdom played an important part in this multinational trial, contributing the largest number of participants. And the results of the TWIST trial informed the most recent UK stroke guidelines, published in 2023, which stated that the benefit of clot-busting treatment for wake-up stroke with the clot-buster tenecteplase was not demonstrated in patients selected by non-contrast CT imaging."
However it remains important for patients who wake up with stroke to seek urgent medical attention, as they may be eligible for clot-busting treatment based on information from more advanced MRI or CT imaging.Professor Thompson Robinson, Lead investigator for the UK arm of TWIST
"Urgent assessment in a specialist stroke service is essential to ensure access to treatment to improve outcome and to reduce death and long-term disability following stroke. BHF continues to fund trials that test treatments to improve outcomes from this devastating condition.”
Study details
"Tenecteplase in Wake-up Ischaemic Stroke Trial (TWIST)"
Award reference: CS/17/5/32826
Chief Investigator: Professor Ellisiv Mathiesen, University Hospital of North Norway
UK Principal Investigator: Professor Thompson Robinson, University of Leicester
Trial registration number: ISRCTN10601890 / EudraCT 2014-000096-80 / NCT03181360
Publication details
Safety and efficacy of tenecteplase in patients with wake-up stroke assessed by non-contrast CT (TWIST): a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2023 Feb;22(2):117-126

