Stroke - RESTART
Should antiplatelet drugs be restarted after a haemorrhagic stroke?
The question
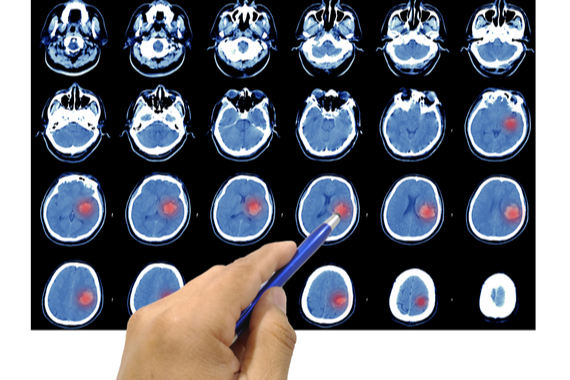
A brain haemorrhage is a type of stroke caused by bleeding into the brain. More than one third of adults who have a brain haemorrhage are taking drugs to help prevent blood clotting, known as antiplatelet drugs, at the time of the stroke.
This is because they may have previously experienced other heart and circulatory conditions caused by blockages in blood flow by blood clots, such as a heart attack or ischaemic stroke. Doctors will usually prescribe antiplatelet drugs, such as aspirin, to try to prevent these conditions from happening again.
Immediately after a brain haemorrhage, doctors will stop prescribing aspirin, because of the risk of further bleeding into the brain. But when patients begin to recover, they and their doctors are often uncertain about whether to restart antiplatelet drugs. Should these drugs be avoided in case they increase the risk of a brain haemorrhage happening again? Or is the risk of another haemorrhagic stroke outweighed by the benefit of preventing conditions caused by blood clots? Professor Rustam Al-Shahi Salman and his team at the University of Edinburgh carried out the REstart or STop Antithrombotics Randomised Trial (RESTART) to find out.
What did the study involve?
Between 2013 and 2018, RESTART recruited 537 participants, who had been taking drugs like aspirin at the time of having a brain haemorrhage. They were randomly assigned to either:
- Restart antiplatelet therapy within 24 hours. This was one or more of aspirin, dipyridamole or clopidogrel, based on the decision of their doctor.
- Avoid antiplatelet therapy.
Participants were followed up over the next 5 years, with the average length of follow-up across all participants being about 2 years. This was done by sending regular postal questionnaires to participants (or their carers) and their GPs. The investigators used this information and medical records to determine if:
- They experienced another brain haemorrhage.
- They had a major bleeding event elsewhere in the body.
- They experienced a condition caused by a blockage in blood flow, such as a heart attack or ischaemic stroke.
- They died during follow up.
Importantly, participants in either group were able to stop or start antiplatelet therapy during follow up if it was medically necessary.
What did the study find?
The key results are summarised in the below video:
- About half as many people who restarted antiplatelet drugs had another brain haemorrhage in comparison to people who avoided these drugs. There was a small possibility that this might have been a chance result. The risks were certainly much smaller than previously thought.
- The number of participants who experienced a serious blockage in blood flow was similar between the groups.
- Taking antiplatelet therapy reduced the overall risk of experiencing a ‘serious vascular event’. This included non-fatal heart attacks or strokes, or death from any cause related to the circulatory system.
Why is the study important?
Recruiting patients from 122 UK hospitals, RESTART was the first multicentre clinical trial to compare starting and avoiding antiplatelet drugs among survivors of brain haemorrhage. The trial was challenging to complete. Patients are often very unwell after a haemorrhagic stroke, which makes enrolment into a clinical trial challenging. Also, doctors often had firm opinions about whether or not to restart antiplatelet drugs after a brain haemorrhage despite a lack of evidence, and they were sometimes reluctant to take part in the trial. This meant that RESTART did not recruit its target number of participants.
But the results of RESTART challenge the widely held view that people who have had a brain haemorrhage should not take antiplatelet drugs. In fact, the study suggests that these drugs may even help to reduce the risk of a further brain haemorrhage. This now needs to be tested more conclusively in a larger trial. And the RESTART team are continuing to follow up the participants to see if new findings emerge over time.
Professor Salman gave his thoughts after presenting the results at the 2019 European Stroke Conference: “At the moment, people do not know what the right thing to do is. Doctors are hesitant about giving aspirin or aspirin-like drugs to people who have had this type of stroke. UK and European guidelines do not give any recommendation, because there hasn't been enough evidence.”
I think we have confirmed the safety of antiplatelet therapy for survivors of brain haemorrhage with these findings. But more work is now needed to see if aspirin might actually lower the risk of brain bleeds as well as clots.Professor Rustam Salman , Chief Investigator, RESTART
BHF is now funding a larger follow on trial to RESTART, called ASPIRING, which aims to definitively test whether taking an antiplatelet drug after a brain haemorrhage can help to reduce a person's risk of risk of experiencing another major vascular event (such as a heart attack, stroke, or dying due to a clotting or bleeding problem). Find out more about ASPIRING.
Study details
"REstart or STop Antiplatelets Randomised Trial (RESTART)"
Award reference: SP/12/2/29422
Principal Investigator: Professor Rustam Al-Shahi Salman, University of Edinburgh
Trial registration: ISRCTN71907627
Publication details
Effects of antiplatelet therapy after stroke due to intracerebral haemorrhage (RESTART): a randomised, open-label trial. Lancet. 2019;393(10191):2613-2623.

