Angina - CorMicA trial
Can doctors make the diagnosis and improve symptoms for people with microvascular or vasospastic angina?
The clinical question
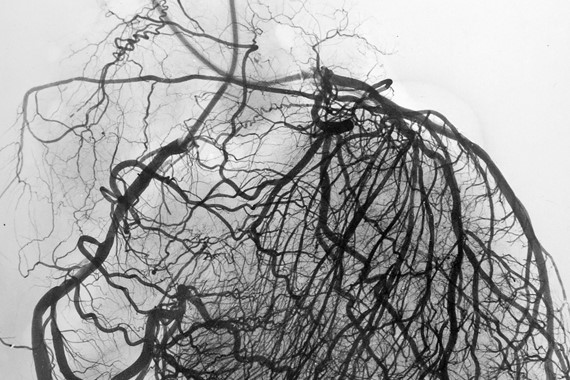
Angina is chest pain that happens when there is a restriction in blood flow to the heart muscle. An x-ray procedure called a coronary angiogram can help to show if there are any blockages in the coronary arteries supplying blood to the heart which can cause this. But the small vessels in the heart are too tiny to be seen with this imaging test.
This is important because the small vessels help to control blood flow in the heart, and there are many more small vessels than large vessels. This can be seen in the ‘stereoangiogram’ image above (by Dr William Fulton, University of Glasgow) - which provides more detail than a standard coronary angiogram.
Up to half of all coronary angiograms carried out in people with suspected angina chest pain show no blockage in the coronary arteries. But this doesn’t mean that the heart’s blood vessels are normal. In some cases, people with coronary arteries that look normal have problems with the functioning of the heart’s blood vessels. For example, microvascular angina, where the tiny arteries within the heart muscle do not work properly, or vasospastic angina, where a coronary artery may look normal, but can go into spasm and suddenly narrow, causing chest pain.
These functional, or 'non-obstructive' coronary artery problems can cause severe symptoms, affecting people’s quality of life and well-being in the longer term. So testing coronary artery function could potentially allow doctors to treat these disorders and improve prognosis.
But coronary artery functional tests are not routinely performed in clinical practice, as not all hospitals are set up to perform these tests. There is also a lack of information whether diagnosing this type of coronary artery disease improves patient well-being. The BHF-funded CorMicA (British Heart Foundation Coronary Microvascular Angina) trial was devised by Professor Colin Berry and his team to try to fill this evidence gap.
What did the study involve?
Between November 2016 and November 2017, 391 people undergoing a coronary angiogram to investigate angina chest pain at two hospitals in Scotland were enrolled in the study. 151 people whose coronary angiogram showed no blockage in the coronary arteries went on to take part. Around three quarters of the participants were women.
All participants had tests to see how well the blood vessels supplying the heart were functioning. These tests were able to identify four groups:
- Microvascular angina
- Vasospastic angina
- Both microvascular and vasospastic angina
- Normal coronary arteries.
Before performing the additional tests, the researchers randomly split participants into one of two groups:
- The intervention group - The results of the coronary artery functional tests were shared with doctors during the procedure. The doctors then prescribed treatments based on all the available clinical information including the coronary function test results.
- The control group - Here, the results of the functional tests were not revealed to doctors, and participants received care based on their clinical presentation and the results of the coronary angiogram alone.
The researchers then assessed the severity of each participant’s chest pain and their quality of life by asking them to fill in a questionnaire after 6 months.
What did the study show?
- Having the results of functional tests helped doctors make a diagnosis. Clinicians who had access to the functional test results felt more certain of their diagnosis of angina due to a disorder of coronary artery function compared with those who were not shown the results.
- In around 50% of cases, clinicians changed their diagnosis once they’d seen the additional test results.
- They were almost three times more inclined to tailor angina therapy to the specific type of coronary artery functional problem diagnosed by the extra tests.
- There were no serious side effects noted in the study.
- People in the intervention group had a significant reduction in the severity of angina and an improved quality of life at 6 months compared with the control group. They had fewer episodes of angina and were able to walk further without being limited by chest pain.
- These findings were maintained during longer term follow-up to 1 year.
Why is the study important?
The CorMicA study reminds doctors to listen to their patients and consider that angina is not always excluded after a ‘normal’ coronary angiogram. Performing functional tests during an angiogram can help doctors make treatment decisions. And prescribing treatments based on these functional tests seemed to benefit patients too.
Dr Tom Ford (first author of the study) presented the results as Late Breaking Science at the 2018 Transcatheter Cardiovascular Therapeutics meeting in San Diego, California. He pointed out that:
This is the first randomised, controlled trial of an invasive diagnostic strategy in angina and non-obstructive coronary artery disease - and it showed that doing additional functional testing is routinely feasible.Dr Tom Ford, lead author CorMicA study ,
While Dr Ford noted that the study wasn’t set up to show exactly why patients in the intervention group improved, he proposed several possibilities: "First, we've given patients a diagnosis; they have an explanation of the symptoms. That's why they came to us in the first place. The other thing is, we've tailored the therapy, so we're treating a specific disorder."
Professor Colin Berry, chief Investigator of the study concluded that: “This was a proof-of-concept study, which we believe provides a basis for carrying out a large, multi-centre trial”.
The participant voice
Mirren Robertson began suffering from chest pain and breathlessness in 2016 while she was on holiday, and went to see her GP. Thinking it might be angina, he prescribed medication - but it didn’t seem to help. So Mirren was sent for further tests at the Golden Jubilee National Hospital, where she was offered the opportunity to take part in CorMicA.
As a result of tests during the trial, she was diagnosed with microvascular angina. Mirren shared her experience as part of BHF Scotland's Bias and Biology briefing in November 2019.
Study details
“BHF CorMicA (British Heart Foundation Coronary Microvascular Angina) trial”
Award reference: PG/17/253288, RE/13/5/30177
Principal Investigator: Professor Colin Berry, University of Glasgow
Trial registration number: NCT03193294
Publication details
Ford TJ, Stanley B, Good R, et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. J Am Coll Cardiol. 2018;72(23 Pt A):2841-2855.

