Stroke - ATTEST-2
Which clot-busting drug should be used to treat an ischaemic stroke?
The clinical question
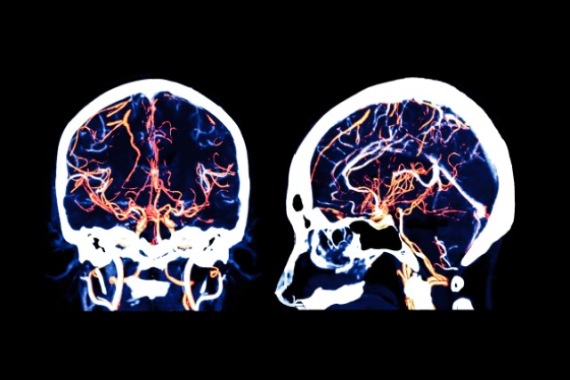
An ischaemic stroke is caused by a blockage, usually a blot clot, cutting off the blood supply to the brain. If patients are given ‘clot busting’ drug treatment in the first few hours after the onset of an ischaemic stroke, their chances of recovery are greatly improved. And the quicker a clot buster can be given, the greater the benefit.
Currently a drug called alteplase is used as the standard clot busting drug for people with stroke. But newer clot busting drugs have been developed, and have already replaced alteplase in other fields of medicine. One of these drugs is called tenecteplase.
Tenecteplase has been tested in small studies for its use in stroke patients. It is easier to give to patients than alteplase, as it can be given as a single injection into a vein whereas alteplase is given as a single injection followed by a 1 hour infusion into a vein — which takes longer and is more complicated to administer.
The ATTEST-2 trial was funded by the British Heart Foundation in partnership with the Stroke Association to compare tenecteplase with alteplase in a large trial in stroke patients. The researchers wanted to find out whether tenecteplase is at least as good as, or better than, alteplase when given to stroke patients.
What did the study involve?
Between January 2017 and May 2023, 1,858 patients were recruited into the trial at 39 hospitals across the UK. To enter into the trial, participants had to be able to receive a clot busting drug within 4.5 hours of the stroke happening.
Participants were randomly assigned to be given either:
- The clot busting drug, tenecteplase, as a one-off injection into a vein
- The currently used clot busting drug, alteplase, given as an injection followed by administration into a vein over 1 hour.
After being randomised, some participants didn’t receive any clot busting treatment, either because an imaging scan taken after they were randomised showed a bleed into the brain (which is a contradiction to a clot buster) or because they rapidly recovered or their blood pressure exceeded the level allowed for clot busting treatment.
In total 1,777 patients received either tenecteplase or alteplase - 885 were given tenecteplase and 892 alteplase.
All participants could have endovascular thrombectomy – where a catheter is placed into the brain to remove the clot that is causing the stroke – if recommended by their clinical team.
At 90 days after entering the trial, members of the trial team interviewed participants by telephone to collect information about how they had recovered after the stroke, using the modified Rankin Scale (mRS). The scale measures the amount of disability caused by a stroke. For example, participants were asked if they could perform their usual daily activities, if they needed help with walking or if they were bed bound, and were given a score for each answer. The scores were added up to give a total for each person — the lower the score, the better the patient’s recovery.
The team then compared the spread of mRS scores for all participants in each arm of the trial and also recorded the percentage of patients in each arm who had lower versus higher mRS scores. They also compared the percentage of participants in each arm who achieved an excellent recovery (with mRS scores of 0–1) with the percentage with a less good recovery (mRS scores of 2-6).
What did the study show?
The trial was interrupted by the Covid-19 pandemic, which halted recruitment for several months and delayed follow up. The average age of participants was 70 years old, 12.4% of participants underwent thrombectomy.
- The overall chances of recovery, measured by the mRS, was found to be no different between tenecteplase and alteplase.
- The proportion of patients achieving an excellent neurological recovery with tenecteplase was also similar to alteplase.
- The number of patients who died or had bleeding in the brain was also similar for both drugs.
- Overall, the results showed that tenecteplase was at least as good as alteplase in helping patients recover from an ischaemic stroke.
- When the results from ATTEST-2 were combined with other trials, the results suggested that there were better outcomes for recovery for stroke patients with tenecteplase compared with alteplase.
Why is the study important?
ATTEST-2 is the largest trial so far that has compared tenecteplase with alteplase in ischaemic stroke, and its finding that tenecteplase is as good as alteplase in helping people in their recovery has important implications for stroke patients and the NHS.
Professor Keith Muir, Chief Investigator of ATTEST-2 explained further: "Tenecteplase has important practical advantages, including being easier and quicker to administer. For instance, many stroke patients have to be moved between hospitals for thrombectomy treatment. Currently, the clinical team has to supervise and deliver the infusion of clot-busting treatment while people are being transferred by ambulance. This can lead to delays in transfers for thrombectomy."
Because tenecteplase is given as a single injection, you give the entire dose immediately, avoiding these logistical challenges. The quicker you can get things done, the better the likelihood of recovery.”Professor Keith Muir, Chief Investigator, ATTEST-2
The ATTEST-2 trial has already changed clinical guidelines. In July 2024, the National Institute of Health and Care Excellence (NICE) recommended that tenecteplase could be used as an alternative option to alteplase, based in part on the preliminary results of ATTEST-2. As tenecteplase costs less than alteplase, NICE has also said its use could potentially save the NHS “millions”.
Study details
Sixth joint Stroke Association/BHF grant: Alteplase-Tenecteplase Trial Evaluation for Stroke Thrombolysis (ATTEST) (seventh call)
Award reference: CS/15/8/32065
Chief Investigator: Professor Keith Muir, University of Glasgow
Trial registration number: NCT02814409
Publication details
Tenecteplase versus alteplase for acute stroke within 4·5 h of onset (ATTEST-2): a randomised, parallel group, open-label trial. Lancet Neurol.2024 Nov; 23(11):1087-1096

