
Between 2015 and 2018, we funded a £1.5 million programme to offer a new way of delivering person-centred care for people with long-term heart and circulatory conditions (LTCs).
The initiative provided better quality care for people with heart and circulatory LTCs, and had a positive impact for healthcare professionals. Importantly, we have added to the evidence base that shows care and support planning can be implemented at practice, community and health system level for multiple long-term conditions.
Now, we need your help to turn this vision into a reality.
The rise of long-term conditions
We are all living longer thanks to advances in treatment, research, care provision and public health. But with greater longevity has come a rise in LTCs.
By 2025, the number of people living with one or more serious LTCs in the UK will increase by nearly one million, from 8.2 million to 9.1 million.1
The traditional care model, reliant on one-off episodes of care, often in acute settings, does not routinely provide the holistic care that best supports people living with LTCs for years or even decades.2-4
Holistic support can reduce unnecessary hospital admissions and improve wellbeing. It is widely recognised that people wish to be more involved in their care and that services need to be better integrated to support them.5,6
Equal partners in care
The British Heart Foundation (BHF) wants to help this vision become a reality. Between 2015 and 2018, we funded five health communities across England and Scotland to offer a new way of delivering person-centred care for people with heart and circulatory LTCs.
This new approach is called care and support planning, a model pioneered by the Year of Care Partnerships. It sees healthcare professionals and people with LTCs come together as equal partners.
Central to this is a collaborative conversation to discuss what matters to the individual and work out the care and support from which they might benefit.
A new approach
Our programme encouraged the adoption of care and support planning using the House of Care, a framework describing what needs to be in place to undertake those conversations.
The BHF programme was established to build on learning from the Year of Care programme in diabetes.7 The BHF programme tested the hypothesis that a person-centred approach to heart and circulatory disease – deploying care and support planning via the House of Care framework – can provide better quality care.
The five health communities each have populations of 50,000 people or more. In England, these were NHS Hardwick Clinical Commissioning Group (CCG) and NHS Gateshead CCG.a In Scotland, the sites were in NHS Greater Glasgow and Clyde, NHS Tayside and NHS Lothian (in collaboration with the Thistle Foundation), with national programme support from the Health and Social Care Alliance Scotland and the Scottish Government.
BHF funding ended in March 2018 and the programme has been independently evaluated by ICF International using a combination of self-evaluation by sites and interviews with patients, healthcare professionals and key stakeholders from each site.8
Highlights
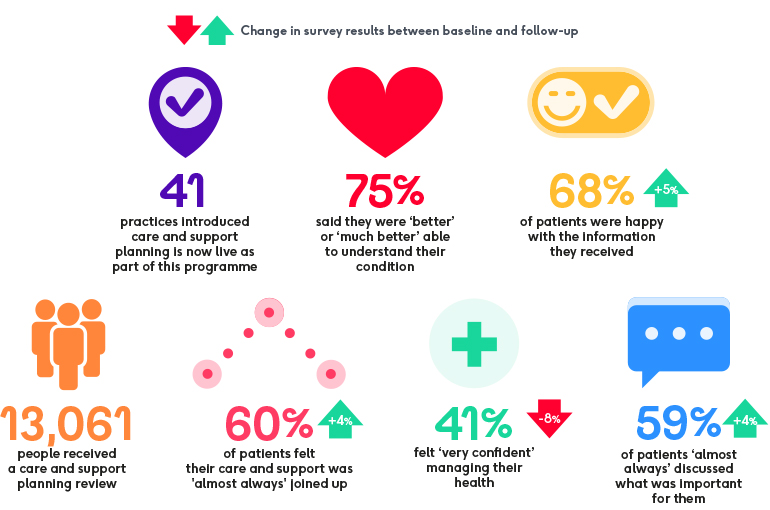
Source: Patient survey results at follow-up (after care and support planning had been embedded in sites), compared to surveys at baseline (when sites were establishing care and support planning). '75%' result baseline data only. For full data and limitations, see the programme evaluation report. References 9-14.
A lasting legacy
Overall, 41 general practices across the five sites have successfully introduced a care and support planning approach as part of our programme. All sites have made sustainable shifts towards person-centred care.
The programme met its aim of providing better quality care for people with heart and circulatory LTCs. We were encouraged to see that the move towards care and support planning also had a positive impact for healthcare professionals.
Experience to date suggests that extending the approach to multiple LTCs could further enhance the patient experience, reduce costs and save time through improved working practices.
On the following web pages we share findings from the final independent evaluation of the programme, consider the legacy for participating sites and summarise key lessons learned for future implementation.
Thank you
The BHF would like to thank the Year of Care Partnerships, Health and Social Care Alliance Scotland, ICF Consulting, members of the Steering and Legacy Committees for the programme, and all healthcare professionals and patients involved in delivering this programme.
References
a NHS Gateshead and NHS Newcastle CCGs merged in 2015. The evaluation focuses only on work in Gateshead as this was a single site at the time of funding.
b 41 practices were specifically included as part of the BHF programme and the evaluation, but more practices have adopted the approach across these five sites.
c Lower confidence was linked to factors such as uncertainty over what results meant or stress/anxiety about being more involved in the conversation. Further encouragement to boost confidence to self-manage with support may be needed. See Improved Care for more.
1 Royal College of General Practitioners (2016). Responding to the needs of patients with multimorbidity: A vision for general practice.
2 House of Commons Health Committee, 2014. Managing the care of people with long-term conditions.
3 Royal College of General Practitioners, 2011. Care Planning: Improving the Lives of People with Long Term Conditions: A summary. RCGP, London.
4 Baird, B. et al. (2016) Understanding pressures in general practice. The King’s Fund.
5 Coulter, A. et al. 2013. Delivering better services for people with long-term conditions: Building the House of Care. King’s Fund, London.
6 National Voices, 2013. A Narrative for Person-Centred Coordinated Care.
7 Year of Care, 2011. Year of Care Report of findings from the pilot programme.
8 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report
9 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report, page 8
10 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report, page 60, Table 8.4
11 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report, page 60, Table 8.5
12 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report, page 61, Table 8.6
13 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report, page 62, Table 8.8
14 ICF Consulting Ltd, 2018. House of Care Evaluation: Final Report, page 61, Table 8.7


